TL;DR:
We’re testing whether a scalable, digitally-supported, community-based Kangaroo Mother Care model delivered through Dimagi's Connect platform can meaningfully reduce neonatal mortality among small and vulnerable newborns. Early results from Uganda are promising and there is strong interest from local implementers in Nigeria. Marginal funding now would support additional newborns in Uganda, let us expand to Nigeria, and generate the evidence needed to assess key uncertainties to determine whether this model should be scaled widely or be deprioritized.
SUMMARY
- Problem: Neonatal mortality remains high (~2.3M deaths/year globally), and premature and low-birthweight babies account for a large share of preventable deaths. Post-discharge care is especially neglected, with Kangaroo Mother Care (KMC) coverage estimated below 5% in many countries.
- Intervention: Structured, verified home visits supporting skin-to-skin care, breastfeeding, thermal regulation, and danger-sign screening. Enrollment typically occurs at facilities, but most care happens at home.
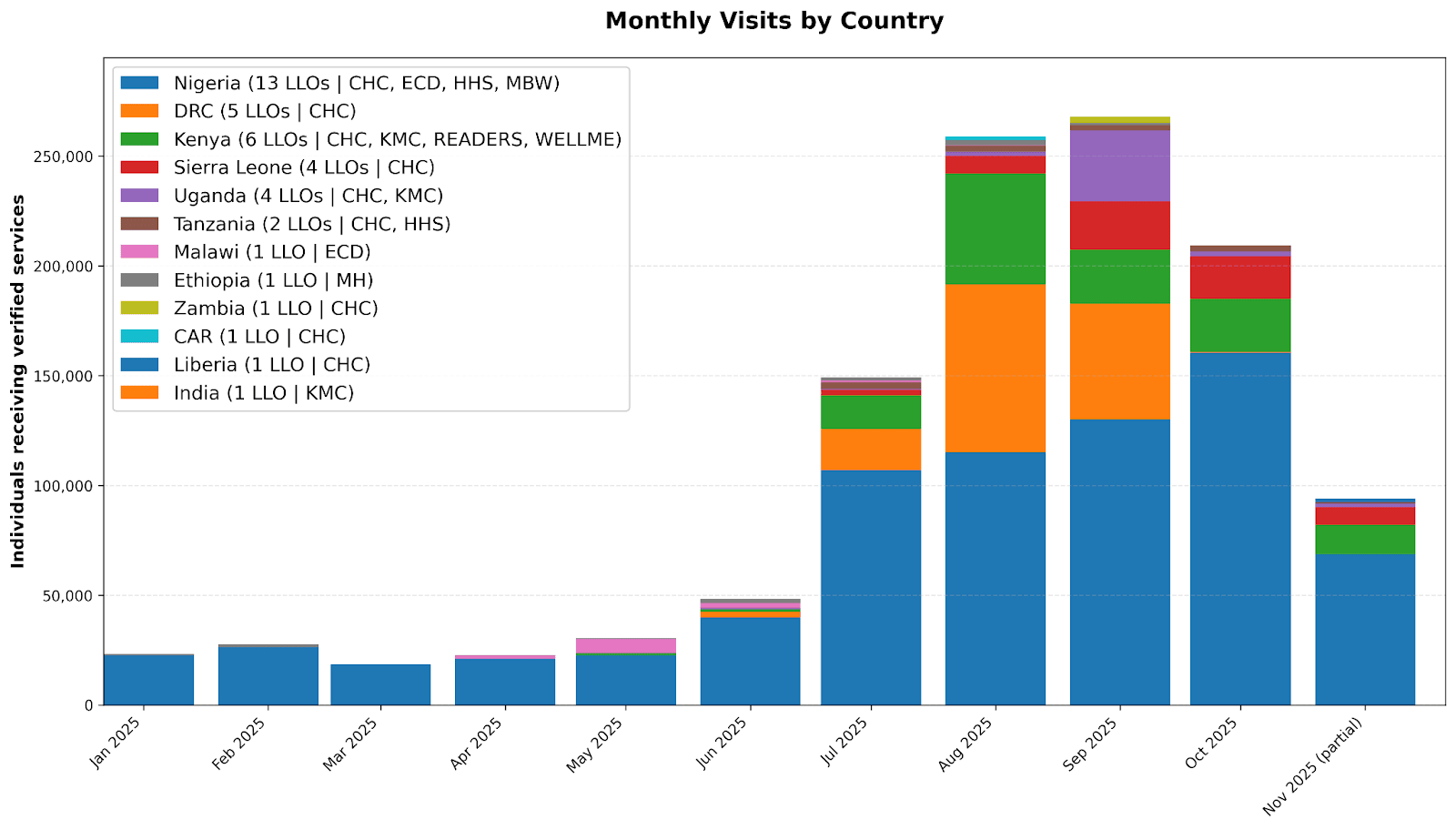
- Platform: Dimagi's Connect digital platform enables local implementers to deliver verified health services at scale (>1M household visits delivered this year by 40+ small local orgs in 12 countries), using a pay-for-performance model that allows rapid replication once an intervention is developed on the platform.
- Why this may scale fast: facility-based KMC requires busy hospital teams to take on new responsibilities and adapt already constrained infrastructure. Community-based KMC, by contrast, adds low-cost capacity through locally-led organization (LLOs) and frontline workers FLWs and extends the reach of existing health services. If validated, it could be rapidly replicated across Connect’s LLO network in multiple countries.
- Traction: Early implementation with Ugandan partners shows strong feasibility, many promising signs of impact, and encouraging MoH engagement.
- Cost-effectiveness: We’re cautiously optimistic given lost cost and ability to focus on babies with high counterfactual mortality. However, there are many uncertainties, including baseline post-discharge mortality for small and vulnerable newborns (SVNs), the mortality reduction achieved through home visits, and full accounting of delivery costs.
- Funding opportunities:
- $4M: expand throughout Uganda to ~50,000 SVNs, conduct operational research, contribute to shift in health system to focus more on SVN care
- $250k: launch in Nigeria where 25 LLOs applied to implement the intervention
- $36 per SVN: delivery cost in Uganda for one of our partners (You can make a direct contribution at our website.)
- Why now? Our current funding covers supporting only about 5,000 more SVNs in a few areas in Uganda and initial small-scale testing in Kenya. Additional funding will preserve momentum and allow us to more fully test the scalability and cost-effectiveness of the model in additional high neonatal mortality countries.
- Why this might not work: We are not yet sure we understand the full costs of the intervention, including transport costs and other services provided by our partners, such as nutrition supplementation for mothers. We have not yet tested whether this intervention can be adopted by a wide range of LLOs.
Additional Background
Kangaroo Mother Care (KMC)
Every year, an estimated 2.3 million newborns die during the first 28 days of life, accounting for nearly half of all deaths in children under five. Most of these deaths occur among babies born too small or too early, with 80% having a low birth weight and two-thirds born preterm. Intervening in this critical neonatal period has huge potential for reductions in child mortality, especially when interventions are targeted towards small vulnerable newborns (SVNs). One of the most proven ways to reduce neonatal mortality among SVNs is Kangaroo Mother Care (KMC), a simple, evidence-based practice involving continuous skin-to-skin contact, exclusive breastfeeding, and early discharge from facilities with close follow-up for both the mother and baby. Evidence consistently shows that compared to conventional care standards, KMC can reduce neonatal mortality by up to 40%, while also lowering rates of infection and increasing rates of exclusive breastfeeding.
There are many barriers that prevent widespread adoption of facility-based KMC. Many SVNs are discharged from health facilities with little support, and caregivers face overwhelming demands to sustain KMC at home without guidance. Health systems often lack the capacity for postnatal follow-up, leaving a critical gap in care. Studies show that community-based support can close this gap: an RCT in India found a 29% drop in neonatal mortality from community-initiated KMC.
Connect
Connect is a digital platform that enables efficient and verifiable delivery of high-impact interventions almost anywhere in the world through local implementers. FLWs are equipped with Connect mobile apps that capture data used to verify each visit including GPS, photo, and timestamp data. Dimagi scaled Connect substantially in 2025 across many interventions, locally-led organizations (LLOs), and countries, as shown in the figure below. We have received $3.5m+ in funding from GiveWell and Founders Pledge, delivering over 1 million visits to date this year, and are scaling down only due to having efficiently disbursed nearly all of that funding.
Connect for KMC
Connect KMC is one of the interventions deployed on Connect. It is a digitally-enabled, community-based model that pays FLWs to conduct structured home visits to support adoption of community based KMC practices for SVNs and initiate appropriate referral to health facilities when needed. Core Components of the Connect KMC Model include the following:
Local Partnerships: Dimagi contracts qualified LLOs with strong community ties. LLOs are responsible for program implementation, including staff recruitment, training, and coordination with local health systems. FLWs are trained on KMC practices and equipped with the Connect KMC mobile app.
Facility Linkages: LLOs work with health facilities to identify eligible SVNs. The caregiver may be enrolled in Connect KMC at the hospital, or the FLWs may go to their homes after discharge. This close link to the facilities also enables referral pathways to the facility when SVNs need care.
Home-Based Service Delivery: FLWs conduct a defined series of in-home visits to support caregivers in adopting and sustaining KMC skin to skin care, monitor newborn health, assess for danger signs, and promote exclusive breastfeeding. The Connect KMC app provides structured guidance for each home visit, including counseling protocols, assessment checklists, and educational materials.
Contracting & Performance-Based Payment: Dimagi establishes contracts with LLOs that include an initial setup fee and fixed payments per verified completed case. Payments are based on visit data captured through the app, and LLOs then compensate FLWs for completed visits
Highlights from Current Pilots
In 2025, we have validated the feasibility of Connect-KMC identifying, enrolling, and providing digitally-enabled follow-up home visits to SVNs and their caregivers. Early implementation shows that LLOs can develop strong relationships with facilities, and that FLWs can effectively deliver follow-up services using the Connect apps as both a job aid and a verification tool.
To date, three LLOs have been engaged, two in Uganda and one in Kenya. One in Uganda has now committed to delivering Connect-KMC to an additional 4,000 SVNs in the next year, expanding from Central Uganda into Eastern Uganda. The other in Uganda has committed to 1,000 additional SVNs once the next app version is finalized.
Government engagement has been strong. Senior Ministry of Health officials have highlighted the gap in post-discharge follow-up care and expressed enthusiasm for the program. They see community KMC as a high-leverage gap in national newborn survival strategies and are interested in developing guidelines informed by the Connect-KMC model.
What Next
We are excited about this work because community-based KMC fits well into Connect’s model for rapid, verifiable scale. Connect has shown that once an intervention is fully developed on the platform - meaning we have clear workflows, training, digital verification, and a pay-for-performance structure - we can replicate it quickly across many LLOs in different countries. Over the past year, Connect supported more than 1.3 million verified household visits across 40+ of organizations and 6 interventions, demonstrating that this infrastructure can absorb and scale new programs with impressive speed. Community-based KMC has many of the same characteristics that have made other Connect interventions scalable: it is a lightweight, protocolized set of activities; it relies on well-defined visit schedules; and it can be delivered by local FLWs with modest training and high accountability. If community-based KMC proves effective, and moreover, cost-effective, we believe we can move from a handful of pilots to multi-country replication faster than is typical in global health, leveraging the exact same mechanisms that allowed Connect to scale other interventions so quickly.
Connect-KMC will generate implementation data around whether home-based KMC can be delivered reliably at scale, whether mothers maintain sufficient skin-to-skin contact without intensive clinical supervision, whether early post-discharge follow-up is feasible, and whether mortality effects observed in facilities translate into community settings. Our digital verification, GPS, photos, timestamps, structured protocols, provides direct evidence of adherence, visit frequency, and continuity of care. If Connect-KMC is scaled across multiple LLOs and regions, the data generated will be comparable, allowing evaluation of cost and outcomes across settings.
Key uncertainties do remain about true baseline post-discharge mortality, the mortality reduction achievable through home-visit support, and the cost structure at scale, especially the balance between transportation, supervision, and FLW caseloads. We also need to understand how well the model works across a broader set of implementers and ensure the intervention design is stable before moving to a rigorous evaluation.
Here are three ways additional funding could accelerate learning and reach more SVNs:
- Expand in Uganda (~$4M): Scale to ~50,000 SVNs across most sub-regions, test the model with a wider range of implementers, deepen MoH engagement, and generate the operational and cost data needed to understand whether this can scale sustainably.
- Launch in Nigeria (~$250k): Twenty-five locally led organizations have expressed interest. A launch would test replicability in a very different health system and provide early feasibility and cost signals outside East Africa.
- Direct support (~$36 per SVN): Fund delivery costs to immediately serve more newborns. This expands reach but does not fund the learning agenda, so works best alongside Option 1 or 2.
Learn more and donate: Connect KMC
Connect: egeoffroy@dimagi.com
