This research project was commissioned by Flourishing Minds Fund and created by CEARCH. It consisted of a review of the available literature on mental health and consultation with over a dozen experts in the field. The full report can be found here.
Structure
- Treatment interventions
- Interpersonal Group Therapy (IPT-G)
- Self-administered & tech-based psychotherapy
- Antidepressants
- Pain mitigation
- Prevention interventions
- Cash transfers
- Alcohol
- Intimate Partner Violence (IPV) (mass media campaign)
- Physical activity campaign
- Diabetes (sugar-sweetened beverage tax advocacy)
- Unwanted pregnancy
- Early-life intervention
- Suicide prevention
- Pesticide bans
- Lithium supplementation
- Intervention BOTECs
Treatment Interventions
Key Findings
- LMICs are generally the best target for treatment interventions due to the lower costs of operating and higher rates of unmet needs
- The quality of psychotherapy studies is highly variable, and many of the observed effects may be the product of bias.
- Interpersonal Group Therapy (IGT) appears to be a cheap way of scaling up mental health provision in LMICs. The persistence and spillover effects are important but not well understood
- Psychotherapy delivered online, by AI or through apps has the potential to be far cheaper than in person, although this is a very young field
- Expanding antidepressant access could be highly effective in some countries, but we have not found examples of past success to learn from
- Severe or chronic pain is often left untreated in LMICs, but increasing opiate access comes with significant risks
In-person psychotherapy
Summary
- No single type of psychotherapy appears to be superior, and effect sizes are relatively independent from the quality of the therapist or the number of sessions
- There are concerning signs of publication bias, response bias and undetected placebo effects in the literature on psychotherapy, which are difficult to adjust for
- Interpersonal group therapy (IGT) in poor countries is cheaper and likely to be more cost-effective than other types of in-person psychotherapy.
- The persistence of the benefits and the scale of spillovers are not well-known, and would benefit from further study
- Driving down cost is probably the best lever for improving the cost-effectiveness of psychotherapy
Effectiveness
There are various types of psychotherapy, including psychoanalysis, cognitive behavioral therapy (CBT) and humanistic therapy. Psychotherapies are used to tackle many mental health disorders, especially depression and anxiety, which together account for over half of the global burden from mental disorders (IHME).
The evidence does not point to a single “best” form of psychotherapy (SoGive, 2023), and so we suggest that the style of psychotherapy is less important than other factors like the cost of delivery.
A number of attempts have been made to determine the average effect size of psychotherapy in general. In a meta-analytic evaluation of meta-analyses (2022), Leichsenring et al. found a modest standardized mean difference (SMD) of 0.34 (95% CI: 0.26-0.42) for psychotherapies compared with placebo or treatment as usual (across disorders). A recent meta-analysis by SoGive (2023) found an effect size of g=0.32 for 6-session psychotherapy interventions for depression.
It is important that psychotherapies are compared with adequate controls and not a theoretical “no change” group, given that control groups tend to show considerable improvement from baseline[1]. Leichsenring et al. found that among patients suffering from depression, subjects in control groups achieved remission in 23% and 33% of cases when they were assigned no treatment or treatment-as-usual, respectively. The figure for those receiving psychotherapy was not much higher, at 43%.
The effectiveness of mental health treatments is often given in “SD-years” of the metric being measured. Hence psychotherapy effect sizes are often given in terms of SD-years of depressive symptoms, where one SD-year is equivalent to reducing someone’s depressive symptoms by one standard deviation for one year. Hence it is not just the initial effect size that matters, but also the persistence of the effects. Mitigating mental illness is thought to have positive effects on people close to the beneficiary, known as spillover effects. The overall effect size of a psychotherapy is thus highly contingent on three factors:
- Initial effect size: the improvement in symptoms at the end of the course of treatment.
- Persistence: the duration of the effects, which is determined by the rate at which the effects decay over time
- Spillover effects: the benefits experienced by those close to the recipient (usually those in the same household)
All studies attempt to measure initial effect size, although these results should be interpreted with caution. Persistence and spillover effects are far less-well understood. If at all, follow-up data is usually collected just a few months after the intervention. Estimates of the long-term persistence of the effects must either extrapolate from short follow-ups, or else rely on a small number of studies with multi-year follow-ups. Happier Lives Institute (2023) found that the exclusion of the five long-term follow-up data points (out of 222 available) decreased the expected persistence of the effects by 58%. Spillover effects are perhaps even more difficult to estimate: there is a small evidence base, and the results are highly heterogeneous.
This suggests that the overall effect size of psychotherapy is not well-understood, and that extra research could be valuable in reducing this uncertainty.
Interpersonal group therapy
Although pioneered in the West, psychotherapy has been shown to be effective in LMIC contexts (Cuijpers et al., 2018). Yet mental health provision in LMICs is generally poor, and very few are able to access psychotherapy. A third of LMICs do not have a mental health budget, and those that do have one spend an average 0.5% of the national health budget on mental health (Founders Pledge, 2019). There are nowhere enough mental health professionals to meet demand: HICs have 50 times more mental health workers per capita than LICs (Founders Pledge, 2019). This makes expert-led psychotherapy an inefficient and insufficient intervention in LMIC contexts.
Interpersonal Group Psychotherapy is a model of therapy that focuses on the individual’s relationships with others (in contrast to CBT, which is more about fostering healthier thought patterns). When delivered by laypeople, IGT can be a scalable and more affordable way of filling the treatment gap - it can cost just $35-650 per person treated (HLI, 2021 i, ii). Local people are given training and run a series of group therapy sessions to people who have been screened for depression or another mental illness. When mental health experts are available, they can be used to train lay-practitioners and to lead projects, in a process known as task-shifting (Patel, 2009). IGT is recommended by the WHO, which has created an open manual for delivering an 8-session program.
Group therapy has been shown to be similar or even greater in effectiveness to individual psychotherapy in treating anxiety and depression (Barkowski et al., 2020, Cuijpers et al., 2019) and was found in one meta-analysis to reduce depression symptoms with a Cohen’s d of 0.63 (95% CI: (0.36, 0.90)) (Cuijpers et al., 2011, mostly HICs). Another meta analysis (2020, mostly HICs) by Janis et al. found improvements in depression scores with Cohen’s d of 0.66 (95% CI: (0.29, 1.03)). This fell to 0.60 in short-term follow-ups and 0.24 after long term follow-ups, suggesting diminishing counterfactual effect over time.
Promising results from a trial in Uganda by Bolton et al. (2003) kick-started interest in IGT in LMICs: “ [a]fter intervention, 6.5% and 54.7% of the intervention and control groups, respectively, met the criteria for major depression compared with 86% and 94%, respectively, prior to intervention”. The benefits appeared to be persistent, with signs of only slight attrition at 6-month follow-up (Bass et al., 2006). However it should be noted that most recipients continued to meet up informally after the intervention (triangle group in the chart below), and only 15% (n=15) did not continue to meet up (square group), which makes the figures on persistence unreliable and perhaps unrepresentative of what would happen in other contexts.
Results from Bass et al. (2006) suggest that IPT-G provided distinct counterfactual benefits compared to treatment as usual (TAU) in Uganda.
It has been argued that “a lot—perhaps too much—hinges on this RCT”.
Concerns about the evidence base
One surprising finding about psychotherapy effect sizes is that they do not seem to be significantly affected by seemingly important factors like the number of sessions, the type of therapy , the mode of delivery and the quality of the therapist. This may reflect an important truth about psychotherapy, or it may suggest that large variations in study quality introduce enough noise to drown out underlying differences in effect size.
Specifically, concerns have been raised that there are signs of publication bias in the literature on psychotherapy, and that studies are often susceptible to response bias and undetected placebo effect. There are established methods for accounting for these effects, but endline results are sensitive to the exact methods chosen. This means that we should interpret all results with caution.
Publication bias
Funnel plots suggest a strong tendency for smaller psychotherapy studies to show larger effect sizes – a sign of publication bias. The extreme nature of the outliers means that publication bias adjustments are extremely sensitive to subjective decisions about which outliers to exclude from the analysis, if any.
The funnel plot below comes from Happier Lives Institute’s psychotherapy meta-analysis, part of their 2023 CEA of StrongMinds. They decided to eliminate all results with an effect size greater than g=2 on the basis that these outliers were probably the result of “poor study quality or statistical noise”. However, as Gregory Lewis points out in a detailed comment, this reduces the publication bias discount enough to lead to a substantially higher effect size than would have been reached had the outliers been included.
However, it is unclear whether keeping the outliers is a better move, since this would make the final results extremely sensitive to the results of a few small, suspicious studies. Overall we urge that readers carefully check publication bias adjustment processes when interpreting estimates for the effect size of psychotherapy.
Response bias
Psychotherapy studies detect mental illness symptoms before and after the intervention by questioning the patient. This exposes them to possible response bias, especially:
- Exaggerating symptoms during screening in order to qualify for treatment
- Exaggerating improvements in their symptoms in order to please the surveyor (social desirability bias)
- Exaggerating improvements in their symptoms in the belief that they may get “cash or material goods” (future hope bias).
In theory, a well-conducted RCT would experience equal amounts of response bias in its control and intervention groups, and hence underlying differences in improvement between the two groups would not be affected. In their 2023 investigation of StrongMinds, SoGive concluded that response bias was probably not a major concern in their meta-analysis, which screens for study quality and accounts for publication bias. GiveWell, on the other hand, discounted effect sizes in HLI’s meta-analysis by 20% to account for response bias.
To us it seems likely that studies with a “waiting list” or “treatment as usual” control group are significantly affected by response bias.
Placebo effect
SoGive (2023) provides a good summary for the evidence of placebo effects in depression studies. The effect size of psychotherapy interventions is generally found to be lower when the control group receives a pill placebo, and placebos perform quite well when compared with passive controls. The placebo effect could explain why the mode of delivery of psychotherapy appears to have little impact on the effect size.
The StrongMinds controversy
StrongMinds is a non-profit founded in 2013 that provides group interpersonal group therapy to impoverished women in Uganda and Zambia, which they now claim to be able to deliver for just $63 per person. StrongMinds has perhaps been assessed more than any other organization providing psychotherapy in LMICs: they were recommended as a top charity by Founders Pledge and Happier Lives Institute (HLI), and these recommendations in turn led to further scrutiny.
We will provide only a brief timeline of the controversy here, but would highlight that the gradual downgrading of StrongMinds’ cost-effectiveness over time appears to be the product of both Optimizer’s Curse and some subconscious bias among those analyzing the organization.
Overall we conclude that StrongMinds is unlikely to be the “holy grail” mental health organization that could rival GiveWell’s top charities. But it remains possible that a cheap and effective psychotherapy intervention can alleviate mental illness for $100s per DALY.
2017
The Oxford Prioritization Project performed a cost-effectiveness analysis of StrongMinds (no longer public), estimating the cost-effectiveness at 154 DALYs per $100,000
2019
Founders Pledge estimated that StrongMinds could avert a DALY for $377 (naively, 265 DALYs per $100,000), and began recommending them as a top mental health charity.
2021
Happier Lives Institute created a cost-effectiveness analysis of StrongMinds that drew upon both general research on psychotherapy and specific data on StrongMinds. They converted mental health improvements into wellbeing improvements, and concluded that StrongMinds could provide 6200 WELLBYs per $100,000. Under certain philosophical assumptions, they argued, this made StrongMinds comparably cost-effective to the best malaria-prevention interventions.
The report was criticized for rushing the meta-analysis process and thereby drawing upon data from interventions that had little in common with StrongMinds. Some commenters accused them of using favorable data on persistence and spillover effects, leading to overestimates of these critical quantities.
2022
Giving What We Can and Founders Pledge were criticized for downplaying the uncertainty around the effectiveness of psychotherapy in general and StrongMinds in particular.
Early 2023
GiveWell released a CEA which applied a similar structure to HLI’s. They used some different inputs and a number of extra discounts to the effect size used by HLI. In a “death by a thousand cuts”, they estimated that StrongMinds was around 4x less cost-effective than HLI had concluded (although still likely more cost-effective than GiveDirectly, a GiveWell-recommended cash transfer charity).
Late 2023
HLI released an updated CEA of StrongMinds that addressed many of the previous criticisms. Lower estimates for effect size and spillover effects decreased the estimated cost-effectiveness. This was partly offset by the decreasing cost per patient of StrongMind’s group therapy, but the final estimate was 3000 WELLBYs per $100,000, around half of their previous estimate.
Although it was a significant improvement on the previous CEA, Gregory Lewis pointed out in a detailed comment that:
- The publication bias discount is extremely sensitive to how outliers are eliminated. HLI appears to have removed outliers in a way that favors StrongMinds. Not removing them would have led to an effect size more than 3x smaller.
- The Bayesian approach taken by HLI places too much confidence in the general effectiveness of psychotherapy, to the extent that it is virtually impossible for StrongMinds-specific data to change the conclusion that the intervention is highly cost-effective.
An RCT on StrongMinds by Baird & Ozler should release its results soon, and the expectation is that it will find a very modest effect size – smaller than the pooled effect size of psychotherapy according to the literature.
Cost-effectiveness of interpersonal group therapy
All of the BOTECs in this report aim to estimate the cost-effectiveness of a hypothetical intervention, using inputs informed by scientific studies and existing organizations. The calculations are found in this spreadsheet which can be run through Carlo to perform a Monte Carlo simulation that provides a distributional cost-effectiveness estimate.
Our interpersonal group therapy BOTEC assumes that an SD-year of depression is worth approximately 0.14 DALYs and finds that there is a 2% chance that IPT-G (modeled on StrongMinds) is more cost-effective than a GiveWell top charity (which we estimate at 737 DALYs per $100,000).
It should be noted that the cost-effectiveness is highly contingent on cost per treatment. We assume that the effect size of the therapy is broadly in line with what has been found in psychotherapy meta-analyses, and that the cost is in line with some IGT-in-LMIC interventions. However, due to the scarcity of high-quality studies of IGT in LMICs, it is possible that these relatively cheap interventions do not yield effect sizes similar to those found in better-studied contexts.
Type | Intervention | Cost-effectiveness compared to cash transfers[2] | Proportion of benefits from mental health |
Psychotherapy | Interpersonal group therapy, LMIC | 5x | 100% |
Sensitivity analysis estimates how much of the variance in the final output is attributable to each of the inputs. It suggests that initial effect size, persistence and cost per treatment are the most important unknowns. Note that we are estimating the cost-effectiveness of a hypothetical IGT intervention, not StrongMinds.
The cost of an intervention is probably far more controllable than the persistence of its effects. For this reason we advise that reducing the cost per treatment is the single best way to increase the cost-effectiveness of psychotherapy interventions. The experts we spoke to suggested that the best ways of reducing costs were 1) avoiding high salaries by headquartering in the target country, and 2) economies of scale. One complication, however, is that monitoring and evaluation add significant costs, and so “cheaper” interventions are more difficult to assess. We feel that funding an RCT on an already-planned program could be a very good way of building the evidence base.
Heuristics for in-person psychotherapy
- Interpersonal group therapy is likely to be cheaper and more scalable than other forms of psychotherapy, especially in LMICs
- Experimental results should be checked for publication bias, response bias and placebo effect
- The best interventions are likely to be longer-lasting than average, with larger positive spillover effects.
- Reducing the cost per treatment is probably the best way of improving psychotherapy interventions. This can be done by avoiding high salaries and by operating efficiently at scale
Self-administered & tech-based psychotherapy
Summary:
- In principle, self-led and tech-delivered psychotherapies can provide most or all of the benefit of in-person therapies at a fraction of the cost
- They come with unique challenges such as low retention rates
- The evidence base is slim but growing: new organizations in the space will provide valuable data
Technology now allows us to deliver psychotherapy remotely. This has the opportunity to be cheaper and more scalable than in-person therapy. Options include:
- Psychotherapy delivered online by video call
- Self-led interventions, usually through a smartphone app
- Chatbot-delivered therapy, which can use conventional or AI chatbot tools
There is evidence that internet-delivered CBT can be effective, and that the effect size is comparable to in-person CBT (Etzelmueller et al., 2020, Ebert et al., 2016, Carlbring et al., 2018). Self-guided internet-based CBT has been found to have a significant effect on depressive symptoms, although the effect is much weaker for those who engage less with the treatment (Karyotaki et al., 2017). There are signs that the gains are still significant 6 months later (Ebert et al., 2016).
High attrition rates are a challenge with online interventions. Among internet-based treatments for psychological disorders “involving minimal therapist contact”, Melville et al. (2010) found dropout rates varying from 2% to 83%, with an average dropout rate of 31% (compared to an estimated 20% in conventional psychotherapy (Swift & Greenberg, 2012)). We suspect that dropout rates are much more variable among online interventions, and that providers of online interventions should have a robust system for minimizing attrition.
The problem of attrition is likely to be worse for self-led interventions. An expert estimated that as few of 1% who download a self-help app end up completing a course of treatment, since the app is competing for attention with all the distractions of a smartphone, and there is no therapist to provide accountability. Self-help interventions have been shown to be effective, but less so than guided interventions (Andersson & Cuijpers, 2009, Baumeister et al., 2014), and we suspect that higher attrition rates account for much of the difference. The expert we spoke to suggested that even if app rights could be acquired for free, high attrition rates can increase marketing costs enough to prevent the intervention being cost-effective. We suspect that self-help apps are high-risk, high-reward options, since apps tend to either attain significant market share or fade into complete obscurity. The counterfactual is important here: self-help apps are a crowded market, so new products must be more effective than the alternatives in order to add value.
There is not much research on chatbot-delivered psychotherapy. An initial study with a non-AI chatbot by Fitzpatrick et al. (2017) suggests a small mitigating effect on depression and anxiety symptoms. AI chatbots such as ChatGPT represent a major step up from earlier chatbots, and we think it is likely that the effectiveness of AI psychotherapy will only increase over time.
There is very little data on the effectiveness of internet-based psychotherapies in LMIC contexts. A meta-analysis by Carter et al. (2020) found mixed results, but the heterogeneity of the studies means that we can not infer much from it. A meta-analysis by Fu et al. (2020) evaluated digital psychological interventions for mental health problems among young people with depression or substance misuse and found “moderate” effect sizes with Hedges’s g 0.60 (vs. control intervention) and 0.54 (vs. treatment as usual).
Poor access to technology is likely to be a barrier in LMICs, especially for targeting older adults. We see stronger potential for targeting young people in LMICs, who are more likely to have a smartphone. For example, it is claimed that about half of children in rural India have access to one.
Online interventions may be less persistent than in-person IGT, where there is potential for lasting, supportive relationships to form, and even the continuation of informal meetings as observed in Bass et al. (2006). However, we think that the constraints on in-person psychotherapy impose a much lower cost-effectiveness ceiling than applies to online interventions. Internet-delivered psychotherapy can rely on cheaper labor from overseas, can bring together geographically disparate people for group interventions, and avoids the cost of hiring venues. Self-help and chatbot interventions do away with many labor costs completely, and have the potential to scale up very quickly.
Kaya Guides is a new organization pioneering a Whatsapp-based guided self-help intervention in India. Their model is to provide minimal levels of human interaction in order to hit a sweet spot between cost and attrition. We think this kind of work is risky, because of the difficulty of gaining share in a competitive app marketplace, but has the potential to be highly cost-effective at scale.
Overcome provides internet-based psychotherapy for mild and moderate mental illness and is free to recipients. It drives down costs by harnessing volunteer labor, chiefly among recent graduates looking for experience to prepare them for a career in clinical psychology. Their main costs are administration and marketing, and the latter is largely covered by Google’s offer of $10k per month in free ads to non-profits.
Overall, we conclude that although it is possible that internet-based psychotherapies have a smaller effect size than in-person alternatives, the opportunities to cut costs mean that they have the potential to be far more cost-effective. Minimizing attrition rates should be a top priority, and internet-based interventions need a sustainable strategy for finding new patients using word-of-mouth or marketing. We have heard anecdotally that staff retention can be a challenge for internet-based psychotherapy, so a sustainable supply of therapists may also be a necessity.
The evidence base is relatively weak, and we think that funding to increase the available evidence could be very useful for the long-term improvement and expansion of internet-based interventions. Funding an existing organization to conduct better M&E or even an RCT could be highly impactful. Important knowledge gaps include the persistence of these interventions, RCTs that directly compare them with in-person interventions, the effectiveness of AI chatbot therapy, and the opportunities for counterfactual impact in crowded markets such as self-help apps.
Cost-effectiveness of internet-delivered psychotherapy
Our BOTEC assesses an intervention along the lines of Overcome, described above.
We estimate that a fully scaled intervention of this type has a 12% chance of being more cost-effective than a GiveWell top charity. Although the evidence base in this field is thin, and our calculations rely on some shaky subjective inputs.
Type | Intervention | Cost-effectiveness compared to cash transfers[2] | Proportion of benefits from mental health |
Psychotherapy | Internet-delivered psychotherapy | 10x | 100% |
Heuristics for self-administered & tech-based psychotherapy
- Psychotherapy can still be effective when delivered online, by a chatbot, or as a self-administered course
- These modes have the potential to offer treatment at a far lower cost
- Low retention rates are a major threat to effectiveness
- This also increases the cost of finding new patients through marketing
- It is harder to reach people without reliable internet access, so these modes are better aimed at the young and those with a smartphone.
Antidepressants
Summary:
- SSRIs can have mild-to-moderate effects on depression
- Access is very poor in LMICs
- Poor infrastructure could be a barrier to extending reliable access to SSRIs within LMICs
Antidepressants have been shown to reduce symptoms of depression. In a meta-analytic evaluation of meta-analyses (2022), Leichsenring et al. found that the effect size of antidepressants on mental disorders was modest and broadly comparable to psychotherapy (standardized mean difference (SMD) of 0.34 (95% CI: 0.26-0.42) for psychotherapies and 0.36 (95% CI: 0.32-0.41) for pharmacotherapies compared with placebo or TAU).
The validity of research on antidepressants has been called into question. Many trials are conducted by scientists with financial conflicts of interest (Perlis et al., 2005). Publication bias is considered to be rampant (Turner et al., 2008). Drugs appear to me more effective when newly released, and become less promising over time, indicative of “novelty bias”. Antidepressants’ strong side effects can undermine blinding in an RCT, and there may be a link between severity of side-effects and estimated effect size (Moncrieff & Middleton, 2018).
Antidepressant use is thought to be 2-4 times higher in HICs compared to LMICs, indicating an unmet need in poor countries (Kazdin et al., 2021). A 2022 study by Rahman et al. spanning 8000 “representative samples” of health facilities in Bangladesh, the Democratic Republic of Congo, Haiti, Nepal, Malawi, Senegal, and Tanzania found that an estimated 8.2% of facilities had amitriptyline and 46.1% had diazepam on the day of assessment (Amitriptyline, an antidepressant, and diazepam, an anxiolytic drug, are classified as essential medications by the WHO).
There are a number of trials exploring the effectiveness of antidepressants in LMICs, but many combine the treatment with psychotherapy and other interventions, which clouds the picture. One such 2010 study in Goa, India, by Patel et al. found that a “psychosocial intervention [plus] antidepressant drugs” was not superior to treatment as usual among private facility attenders, and increased the chance of recovery by 55% among public facility attenders. This is a reminder that the counterfactual quality of treatment is important when considering the benefits of an intervention. A cost-effectiveness study in Nigeria found that older, cheaper antidepressants were significantly more cost-effective than newer, more expensive ones.
There are a number of barriers to successfully improving antidepressant access in poor countries. Shortages of mental health professionals will make diagnoses less accurate, increasing the chances of underprescription for those with severe depression and overprescription for those who are not depressed, as was observed in India (Pillai et al., 2021). Unreliable supplies of medicines at pharmacies and health centers increase the chance that patients will run out of medicine, which can have negative consequences. Poor awareness of mental health will prevent people from seeking help, and people may not identify depression symptoms as a medical issue. Costs can be prohibitive, and the burden of paying for antidepressants may cause more people to cease treatment prematurely.
We suspect that the greatest opportunities for change are in societies where medical infrastructure is relatively strong, and where the causes of antidepressant undersupply can be easily fixed. There may be opportunities to improve government policy or health worker training to ensure that antidepressants are issued when they are needed.
Pain mitigation
Summary:
- Lack of awareness and access may be preventing many in LMICs from getting relief from chronic low-level pain
- Lack of opiate access leads to a huge amount of avoidable severe pain
- Increasing access to pain relief drugs comes with major downsides such as the risk of addiction
Pain is bad, and this badness is probably not fully captured by DALYs and QALYs. Pain may also increase the severity of mental illness: a WHO study found that those experiencing persistent pain were three times likelier to suffer from anxiety and depression than others (AOR: 4.14) (Gureje et al., 1998).
The prevalence of chronic pain in developing countries has been estimated at 18% (Sá et al., 2019), and yet the WHO estimates that over 80% of the global population do not have access to treatments for moderate to severe pain (Morriss & Roques, 2018). 50% of the world’s poorest people receive just 1% of the available opioids (Yao et al., 2023).
The treatment gap for mild pain relief is less extreme. A 2021 scoping review on over-the-counter analgesics (painkillers) in various Sub-Saharan African countries by Kawuma et al. (2021) found that analgesic use “among pregnant women was between 26–78%, students 55– 82%, general community members 38–97% and hospital patients 45–89%”. However, a medical profession working in Uganda suggested to us that arthritis pain, which is very common among the elderly in the country, is severely undertreated.
Increased access to pain medications comes with risk. The GBD survey indicates that the burden of opioid abuse in South Asia and Sub-Saharan Africa is about half the global rate (see graph below, generated at vizhub.healthdata.org/gbd-results/). This is partly thanks to a lack of opiate availability in the medical system: opiate prescription is one of the main pathways to addiction, and medical opiates, when they are available, sometimes end up on the black market. A number of experts we spoke to urged caution when expanding access to opiates because of the danger of addiction and abuse.
Low-level painkillers come with health risks. Even for persistent arthritis pain, the NHS and Mayo Clinic advise only occasional use of painkillers due to the health risks. Nonsteroidal anti-inflammatory drugs (NSAIDs) have been associated with cardiovascular risk (Reddy & Roy, 2013) and peptic ulcers, and are dangerous for people who already have peptic ulcers, which are more prevalent in poor countries (IHME).
The International Association for the Study of Pain (IASP) recommend “[e]ducation, clinical training, and advocacy initiatives” to improve the mitigation of pain in poor countries. The 1-day Essential Pain Management program “is a simple 1-day workshop aimed at teaching a multidisciplinary group to better recognise, assess and treat pain of all types” and has been delivered in many countries since 2011 (Goucke & Morris, 2012).
We think the best opportunities are lower-risk ways of expanding access to pain relief. Better education and training can increase the safe and responsible allocation of pain relief drugs by healthcare professionals. Increasing opiate access for terminal illness carries less risk of addiction and abuse. Increasing painkiller availability is less dangerous in countries that have robust prescription and restriction systems, and it is possible that helping countries to develop better medicine safeguarding controls will make expanding painkiller access safer and more feasible in the future.
Critical research gaps
As explored in the second post in this sequence, mental illness is expected to grow in relative importance this century. As the cost–effectiveness of the best physical health interventions drops, the best mental health interventions will become more appealing. We need:
- Studies with long-follow ups to track the persistence of the benefits from the intervention
- Better evidence on spillover effects on the whole household, including data on wellbeing
- Better ways of minimizing response bias when administering symptom-based questionnaires like the PHQ-9
- Data on the counterfactual impact of pain interventions such as increased medication access and training programs
Conclusion
The vast majority of people in LMICs suffering from mental illness have no access to treatment. This makes the counterfactual impact of providing treatment very strong, but it also throws up barriers. A lack of existing infrastructure means that organizations must plan carefully to ensure that their intervention is feasible in the target country. Interpersonal group therapy has been delivered in a way that is mostly independent from existing mental health provision. Improving antidepressant coverage, however, is probably very difficult to do without a deep understanding of existing health structures.
It remains unknown to what extent mental health problems in poor countries are caused by poverty itself. However, research suggests that patients in LMICs do respond positively to mental health interventions. Much more research is needed to determine just how powerful these interventions are.
Overall we suspect that reducing the cost of treatment is usually the best lever for improving the cost-effectiveness of mental health treatments.
Prevention Interventions
Key Findings
- We can clearly identify risk factors associated with future mental illness, but it is very difficult to establish the strength of causation. This makes prevention interventions more uncertain.
- It is possible that policy advocacy promoting healthier lifestyles could cost-effectively improve mental health by preventing diabetes, obesity and physical inactivity
- It is widely believed that early-life mental health interventions are preferable, but we are not sure whether the preventative power of early interventions outweighs the ease of targeting mental illness in adulthood
- We can reduce the burden of suicide by restricting access to the deadliest methods. Pesticide bans have been highly effective, but the marginal impact of extra funding is unclear
- More research is needed on the counterfactual effects of targeting mental health risks factors
Mental illness risk factors
Mental illness correlates with a number of economic, social and health factors. By targeting these factors we can hope to prevent mental illness before it occurs.
It can be very difficult to determine causation, however. All mental health disorders appear to have genetic components which are difficult to isolate from the effects of parenting and the home environment. Mental illness is linked with self-destructive behavior, traumatic life events, loneliness, unemployment and many other things. But we can’t say for certain how much an improvement in one of these indicators will improve mental health. Furthermore, these indicators tend to be linked with other factors like ancestry, poverty and poor emotional literacy which may be the underlying cause.
Cash transfers to alleviate poverty
Summary:
- Cash transfers appear to have a small but significant positive effect on mental health
- The effects are strongest when people in poverty are the target
- The mental health benefits of cash transfers do not radically alter the cost-effectiveness of CT programs
- We are confident that directly addressing mental health can mitigate mental illness more cost-effectively than cash transfers
Cash transfer programs vary in the scale and style of the payments they provide, but findings generally suggest that “there may be a positive, albeit modest, relationship between cash transfer receipt and improved mental health” (Evans-Lacko et al., 2023). The effect size (for SWB or depression/anxiety) seems to be around 0.1-0.15SD (Ohrnberger et al., 2020, McGuire et al., 2022, Wollburg et al., 2023).
The effect is far weaker when the recipients are not living in poverty (Thompson et al., 2022). Single payments may be preferable to regular payments, and the best CT programs communicate with recipients so that they know how much money to expect, and when. The persistence of mental health improvements is poorly understood and, given the small size of the improvement, difficult to measure. Of four studies that had follow-ups after 2-9 years, effects appear to have approximately halved (Wollburg et al., 2023).
In their analysis of cash transfer programs, Happier Lives Institute (HLI) estimate that a CT program costing $1,274 improves recipients’ mental health (which they equate to SWB) by 0.4 SD-years, or a total of 1.7 SD-years among the whole household (confidence interval (0.40, 5.94)) (HLI, 2022). As a rough comparison, Givewell estimated that just $105 spent on interpersonal group therapy would improve SWB by 1.1 SD-years across the household.
It seems likely that CT programs have positive spillover effects within the household, but it is also possible that there could be negative spillover effects for those who do not receive a cash transfer, who become poorer in relative terms and may feel a sense of injustice. There is little data on this. McGuire et al., 2022 assess four trials that explore non-household spillover effects, of which “[t]wo found negative spillovers but the average effect is not statistically significant and is close to zero.”
Overall it seems very unlikely that cash transfer programs can rival interpersonal group therapy for cost-effectiveness on mental health or wellbeing alone. However, proponents of cash transfers are usually interested in the poverty-alleviating effects. The small positive effect on mental health may make cash transfer programs slightly more appealing than they previously were.
Mental health effects should also be accounted for when considering introducing maternity pay, pensions or UBI for populations in poverty.
Our BOTEC estimates that a campaign to persuade a poor country to implement a child poverty grant (in the style of South Africa’s CSG) has a 46% chance of being more cost-effective than a GiveWell top charity. However, only around 3% of the expected benefits would be from mental health.
Type | Intervention | Cost-effectiveness compared to cash transfers[2] | Proportion of benefits from mental health |
Social support | Child poverty grant advocacy | 30x | 3% |
Our results are highly contingent on the counterfactual value of government spending, of which we are highly uncertain. In short, it is unclear to us how impactful child poverty grants would be in a low-income country compared to the things the government currently spends money on.
Alcohol
Summary:
- The association between alcohol abuse and mental illness is strong
- However, the strength of the causal link is unclear
Alcohol use and abuse is associated with poor mental health. “The prevalence of anxiety, depression, and other psychiatric disorders is much higher among persons with Alcohol Use Disorder (AUD) compared to the general population” (NIH).
Negative spillover effects of alcohol abuse are likely to add to the burden. Dawson et al. (2007) found that “women whose partners had alcohol problems were more likely to experience victimization, injury, mood disorders, anxiety disorders, and being in fair or poor health than women whose partners did not have alcohol problems”. Even after accounting for the women’s increased rate of substance use, odds ratios for the above indicators were 2.1-3.4.
According to the GBD, alcohol use is the largest risk factor for suicide (which forms the vast majority of the burden of “self-harm”), accounting for 15% of the burden.
Percentage of Self-Harm DALYs attributable to top risk factors for both sexes combined (GBD, 2019).
The strength of the causal relationship is difficult to determine, as alcohol is often used as a “coping mechanism” by those suffering from mental illness. We believe that policies that reduce alcohol consumption, and especially abuse of or addiction to alcohol, will improve mental health outcomes.
Intimate Partner Violence (IPV)
- IPV is strongly associated with poor mental health
- Depression will soon overtake HIV/AIDs as the primary health burden associated with IPV
- However, the strength of the causal link is unclear, as there are other possible factors at play
- IPV is notoriously difficult to study and to tackle, although a recent mass media intervention shows early promise
Intimate Partner Violence (IPV) “is defined as any lifetime experience of physical or sexual violence perpetrated by a current or former intimate partner, and is estimated among females only” (IHME).
The data is extremely unreliable due to the difficulty of measuring something that is usually hidden in the home and is a taboo topic. The GBD survey measures IPV as a binary score, so we are unable to differentiate between different types of IPV. According to the GBD, mental disorders are becoming the main source of health burden associated with IPV, as the global burden of HIV/AIDS declines.
Data from GBD study (2019).
IPV is estimated to be responsible for 11.0% (95% UI 0.1–24.0) of DALYs due to depressive disorders among females, increasing each individual’s risk of major depression by an estimated 54%. However, the GBD data implies an extremely low level of certainty on the mental health burden of IPV. The Lower and Upper estimates for the global depression burden attributable to IPV differ by a factor of 500x, which is the highest we have seen for any cause.
IPV is associated with 0.53 suicides (deaths from self-harm) and 1.58 other deaths (presumably at the hands of their partner) for every 100,000 women per year. It has been associated with increased rates of postpartum depression (Beydoun et al., 2012), and may have persistent effects on the children of victims.
Links between IPV and mental health outcomes should be seen as tentative. There are a host of potential confounding factors associated with IPV which may also influence mental health outcomes.
IPV is difficult to prevent. Education programs may be effective, but studies typically measure improvements in knowledge and self-proclaimed beliefs on the subject, not changes in the incidence of IPV, so the effectiveness is unknown. Bettle (2022) suggests that mass media interventions are particularly effective “where unhelpful social norms (such as the acceptability of intimate partner violence) persist”, hypothesizing that funding an IPV mass media campaign could be significantly more cost-effective than donating to GiveWell. Fairless (2023) recommended that Charity Entrepreneurship incubate a charity pioneering an “entertainment-based” mass media intervention to reduce Intimate Partner Violence. They caution that monitoring and evaluation will be a challenge for a sensitive subject “that presents additional challenges for outcome verification.”
Cost-effectiveness of a radio campaign to prevent IPV
Charity Entrepreneurship have identified a radio campaign to combat IPV as a promising idea. Similar campaigns have been delivered by Development Media International and Family Empowerment Media to encourage breastfeeding and contraceptive use in Sub-Saharan Africa. Radio campaigns may be most helpful “where unhelpful social norms (such as the acceptability of intimate partner violence) persist” (Bettle, 2022).
Our BOTEC estimates that a radio campaign to prevent IPV would have a 4% chance of being more cost-effective than a GiveWell top charity. However, it is likely that the GBD, our source for the health impacts of IPV, severely underestimates the full harm associated with IPV. The GBD attempts to capture the increased risk of depression, violent death and injury, and increased HIV transmission associated with IPV, and not stress, shame, fear and pain.
We are also highly uncertain about the cost of the campaign and the power it would have to change perpetrators’ decision-making. We do not attempt to model positive or negative secondary effects. Mitigation of physical impacts constitutes around 70% of the benefit.
Type | Intervention | Cost-effectiveness compared to cash transfers[2] | Proportion of benefits from mental health |
Mass media | Radio campaign to combat Intimate Partner Violence (IPV) | 5x | 30% |
Religion
Summary:
- Religious belief is associated with better mental health, although it is difficult to convert this insight into intervention recommendations
- Religious organizations have several properties which make them well-placed to implement interventions in LMICs
Religious people seem to be more resilient to mental illness (Dein, 2010, LondonGal, 2023). This could be because of strong community support and spiritual practices that encourage positive emotions (Mueller et al, 2001).
Although we don’t endorse encouraging people to be more religious, there are signs that a religiously-aligned organization could be well-placed to improve mental health in deeply religious societies.
- Members of the religious community hold a lot of sway which could be used to increase awareness of mental health. Experts have suggested to us that people in poor countries are less likely to consider mental illness to be a major health problem, and may equate mental illness with conditions like severe schizophrenia, but not depression and anxiety.
- Marketing costs are a potential barrier to online or tech-based psychotherapy interventions. Religious groups may have strong networks which provide “free marketing” and could increase the chances of reaching a wide audience
- People often give to causes within their faith, which could make fundraising easier for a religious organization
- Religious groups often have a tradition of volunteering, which can drive down labor costs.
Many of these points stemmed from a conversation with the founder of Wailing Women, a Christian charity. WW grew a global audience during lockdown through social media, and produced uplifting live events, group events and courses of therapy.
There are a number of reasons to be wary about supporting religious organizations. They may only help people with the same religious affiliation, or they may allocate resources to religious activities with no obvious health or wellbeing benefits. It’s also possible that people giving time and money to religious charities may be manipulated into doing so.
Physical activity
- Physical activity is associated with lower rates of developing depression and less severe symptoms of depression and anxiety, although the direction of causality is unclear
- Government health campaigns may be able to prevent cases of depression by encouraging physical activity
There is an established correlation between physical incidence and both incidence and severity of mental disorders. Schuh et al., 2018 examined 1.8m person-years of data and found that compared with people with low levels of physical activity, those with high levels had lower odds of developing depression (adjusted odds ratio=0.83, 95% CI=0.79). A Systematic Review and Meta-analysis by Pearce et al. (2022) found that “relative to adults not reporting any activity, those accumulating half the recommended volume of physical activity had 18% (95% CI, 13%-23%) lower risk of depression. Adults accumulating the recommended volume had 25% (95% CI, 18%-32%) lower risk with diminishing potential benefits and higher uncertainty observed beyond that exposure level”.
Rebar et al., 2015 is a “meta-meta-analysis of the effect of physical activity on depression and anxiety in non-clinical adult populations”. Physical activity had a moderate effect on depression [standardized mean difference (SMD) = -0.50; 95% CI: -0.93 to -0.06] and a small effect on anxiety (SMD = -0.38; 95% CI: -0.66 to -0.11). An overview of systematic reviews by Singh et al. (2022) found that physical activity had medium effects on depression (median effect size=−0.43, IQR=−0.66 to –0.27) and anxiety (median effect size=−0.42, IQR=−0.66 to –0.26).
These results should be taken with a large grain of salt. Depression is associated with low energy, poor sleep and diminished motivation. It is likely that those experiencing mild or undiagnosed depression are less physically active. When they later cross the threshold to diagnosed depression, this may be attributed to low physical activity rather than their previous state of depression. Exercise is known to improve sleep, and poor sleep is known as a symptom of depression. It could be that some of the observed effects of exercise on depression symptoms stem from sleep improvements rather than improvements in “underlying” depression.
Our BOTEC, which relies on mostly subjective estimates for inputs, estimates that advocacy for a physical activity campaign has a 21% chance of rivaling GiveWell top charities for expected cost-effectiveness. We are very uncertain about the cost-per-person and the effect size of physical activity campaigns, and most of the expected value lies in low-cost, high-effect scenarios.
Type | Intervention | Cost-effectiveness compared to cash transfers[2] | Proportion of benefits from mental health |
Health nudges | Physical activity campaign advocacy | 17x | 17% |
Obesity
A systematic review by Blasco et al. (2020) “confirmed that there is indeed a link between depression and obesity, although there are doubts as to the significance of this relationship.” A A systematic review and meta-analysis of longitudinal studies by Lippino et al. (2010) found that obesity increased the risk of onset of depression (unadjusted OR, 1.55; 95% confidence interval [CI], 1.22-1.98; P < .001), and that the link was stronger for obesity than overweight, suggesting a dose-response relationship. They also found that depression increased the odds of developing obesity (OR, 1.58; 95% CI, 1.33-1.87; P < .001), indicating a two-way relationship.
Diabetes
Diabetes is associated with an increased risk of depression. CEARCH’s cost-effectiveness analysis on policy advocacy for sugar-sweetened beverage taxes (Report, CEA) found that 2-3% of cases of depression globally are linked to diabetes. It estimates that 1.4% of the total burden associated with diabetes comes from death and disability linked with depression and suicide. Even though this is a small fraction of the overall burden, the high expected cost-effectiveness of the intervention may make it an appealing candidate on mental health grounds alone.
These results are highly uncertain because of the difficulties in modeling the tractability and effectiveness of government health policy.
Another weakness is that the causal link between diabetes and depression is not fully established. Two meta-analyses have found significant correlation between diabetes and depression (Chireh et al., 2019, Elamoshy et al., 2018). Diabetes was found to increase the risk of suicide by Wang et al. (2017). The suicide link failed to reach significance in two other studies (Wang et al., 2016, Elamoshy et al., 2018), but with risk ratio of 1.61 and odds ratio of 1.85 respectively.
Our BOTEC estimates a 63% chance that the expected cost-effectiveness of SSB tax advocacy exceeds GiveWell top charities. Only 4% of the benefits would come from improved mental health.
Type | Intervention | Cost-effectiveness compared to cash transfers[2] | Proportion of benefits from mental health |
Health nudges | Sugar-sweetened beverage tax advocacy | 79x | 4% |
Unwanted pregnancy
Increased contraceptive access and family planning education may improve mental health by preventing the negative effects of unplanned pregnancies.
According to Stevenson et al. (2023), “The prevalence of perinatal depression is estimated to be 12–17% and the prevalence of perinatal anxiety is estimated to be 15% globally among the general population”. In a South Korean study, unintended pregnancy was associated with 20-22% greater odds of maternal depression (compared with intended pregnancy) and with higher depression and stress scores (Bahk et al., 2015).
The counterfactual impact of pregnancy on depression may be exaggerated. Pregnant women and mothers have more contact with the healthcare system and may be more likely to be diagnosed with depression. Many studies on perinatal depression rely on survey methods that tend to find higher prevalence rates[3]. It is not clear to what extent pregnancy increases the risk and severity of depression.
Furthermore, studies probably fail to separate the direct effects of unwanted pregnancy from those of other, correlated, factors. In Bahk et al. (2015), much of the increased risk and severity of depression linked with unplanned pregnancy was explained by higher rates of marital conflict and lower rates of father participation.
Our best guess is that preventing unwanted pregnancies would prevent mental illness, but that these benefits would pale in comparison to others (such as reductions in maternal mortality, unsafe abortions and stillbirths (Sully et al., 2019)) and would probably not be cost-effective on their own.
Early-life intervention
Summary:
- Interventions aimed at mothers, babies, children and young adults are believed to have preventative mental health benefits
- However, factors like genetics and poverty cloud the picture, undermining the strength of this claim
- Many mental health conditions emerge in adulthood, making targeting children less efficient
- There are well-known childhood risk factors associated with later mental illness, but evidence-based interventions are lacking
Adult mental illness correlates with perinatal depression, childhood trauma and childhood mental illness. There is a widespread conviction that early-life interventions are therefore preferable to adult interventions, but we believe that this is not always true.
Most mental disorders begin in adolescence or adulthood (Kessler et al., 2007). Mental disorders are typically not diagnosed or treated until years after the symptoms begin, and earlier diagnosis could lead to better outcomes. Kessler et al. (2007) suggest that “[a]s many mental disorders begin in childhood or adolescence, interventions aimed at early detection and treatment might help reduce the persistence or severity of primary disorders and prevent the subsequent onset of secondary disorders”, although “research is needed on treatments of early cases [...] to determine whether this is true.”
It’s possible that tackling childhood risk factors associated with adult mental illness could have long-lasting benefits. A number of key risk factors have strong correlation with adult mental illness, but most studies fail to completely control for the effects of genetics.
Childhood trauma, childhood adversities and childhood sexual abuse are all correlated with poor mental health outcomes in childhood. (McKay et al., 2018) found that exposure to bullying, emotional abuse, maltreatment and parental loss were associated with adult mental disorder, with odds ratios varying from 1.24 to 2.09. Data from the GBD survey suggests that bullying victimization “accounted for 7.1% (2.2–14.4) and 4.6% (1.1–9.6) of YLDs for anxiety disorders and major depressive disorder (MDD), respectively”. Childhood sexual abuse was found to be “responsible for 4.4% (95% UI 2.4–6.8) of global YLDs due to depressive disorders and 9.6% (1.3–22.1) of global YLDs due to alcohol use disorder.” Kessler et al (2010) estimate that eliminating childhood adversities would cause a 30% drop in mental disorders.
We see reasons to be skeptical of these estimates. Child abuse is difficult to measure. When asking parents if a child has been abused, they may have reason to lie to protect the perpetrator. When asking the child, they may be dishonest or they may not know that they have been abused. Even when asking adults whether they were abused as a child, they may be more likely to remember abuse if they believe it affects their mental health as an adult. This not only undermines the correlation data, but hampers feedback loops for any interventions aimed at reducing the incidence of childhood adverse experiences. Furthermore, adverse childhood experiences could be associated with factors such as genetics and poverty which may themselves have causal effects on adult mental illness.
Interestingly, there appears to be a genetic component in the effect that maltreatment has on a child. One study found that holders of the MAOA gene had a much stronger correlation between childhood maltreatment and antisocial behavior (Taylor, et al., 2007).
The earliest interventions target pregnant mothers and mothers of babies. A number of educational programs aimed at mothers and young children appear to have effects on behavior and child development & mental health (Klasen & Crombag, 2012). But data on long-term mental health outcomes is simply not there.
Early adolescence may be a good time to tackle behavioral problems and teach emotional regulation. The evidence is nicely summarized in Javier, 2022, but there is no convincing confirmation that interventions in adolescence have long-term effects.
The key weakness of early-life interventions is that most mental disorders have not yet emerged, so it is difficult to target children accurately. Risk factors can improve targeting, and it is well understood that prioritizing children with risk factors can yield better results (Yu et al., 2023). But targeting before symptoms have emerged can only be so good.
On the other hand, the link between childhood and adult mental health is inherently difficult to study, and we remind readers that absence of evidence is not evidence of absence.
Early-life interventions have a number of strengths. Mothers are relatively easy to reach through medical appointments during pregnancy. Schools provide a convenient platform for educational interventions, and can be a useful ally in early diagnosis of risk factors and mental disorders. It seems possible that policy advocacy could unlock and direct government funding towards youth-targeted mental health prevention work. Javier, 2022 suggests prioritizing “interventions focusing on stress, strengths, values, problem-solving etc.--more familiar terms than mental health.” It seems plausible that such interventions could be integrated into school curricula.
It is not clear whether the pros of pre-emptive early-life interventions outweigh the cons. Early diagnosis, however, would be entirely positive. There may be scope for school or online services that can identify signs of mental illness sooner, and provide treatment several years earlier than it would have been.
Preventing suicide
We think that the top ways of preventing suicides are to treat and avert cases of depression (see Treatment at the top of this post) or to restrict the means of suicide. It is accepted in the field that blocking highly-reliable methods of suicide forces people to turn to less reliable methods and increases their chance of surviving the suicide attempt. The effectiveness of means-restriction depends on how determined to commit suicide the person is. An expert we spoke to split suicide attempts into two categories: those that are the product of persistent, severe depression; and those that result from a passing moment of despair. Means restriction is considered to be effective at preventing the latter, “low-intent” type of suicide.
Famous examples of this effect include the drop in suicides after carbonoxide was removed from the UK gas supply (Kreitman, 1976) and the drop in suicides in response to various pesticide bans in Sri Lanka (Gunnell et al. 2007 & Knipe et al., 2017).
It is uncertain how highly to value an averted suicide, given that suicide is associated with depression and suffering. But we don’t think this uncertainty is one of the main concerns when assessing suicide-prevention measures.
Pesticide bans
Summary
- Millions of people have committed suicide with pesticides since 1960
- Banning the most toxic substances is associated with drops in overall suicide rates
- Progress has been achieved by a small organization in the space
- Most of the best opportunities have been taken, but there is still scope for highly cost-effective gains by targeting smaller countries or by aiding enforcement efforts
During the Green Revolution, highly toxic pesticides became widely used across much of the world. They became a popular means of suicide in poor countries, and are thought to have been used in between 9 and 17 million suicides since 1960[4](Karunarathne et al, 2019).
In Sri Lanka, for example, suicide rates exploded as pesticide use increased across the country. Prof Michael Eddleston of Edinburgh University claims that turning points in the national suicide rate can be attributed to new substance bans[5](Knipe et al., 2017).
Similar but less drastic effects have been observed in Nepal (Utyasheva et al., 2021), India, Taiwan and South Korea (Bonvoisin et al., 2021). In China, pesticide suicides dropped by 60.5% between 2006 and 2018, during which time 12 deadly pesticides were banned or restricted.
One challenge is that most pesticides are somewhat toxic, and so removing one substance causes people to move to another, still toxic, pesticide. Leah Utyasheva and Michael Eddleston of The Centre for Pesticide Suicide Prevention see this as an iterative process where each round of bans helps to identify the substances that should be banned in the next round. They insist this does not continue indefinitely, since controls on new substances have improved over time and hence once all of the worst chemicals from the early days of the Green Revolution have been restricted, the risk becomes very low.
They also believe that most pesticide suicides come from moments of temporary despair and that preventing them often leads to the beneficiary living a normal life.
It has been suggested that banning pesticides can have serious downsides by reducing the agricultural output of poor, food-insecure countries. In a BOTEC, GiveWell subjectively discounted the effectiveness of pesticide bans by 30% to account for decreased agricultural output. Sethi et al. (of which Michael Eddleston was a co-author) claim to have found that the 2011 pesticide bans in India seemed to have “negligible impact” on crop yields on the 2012 harvest, although it seems likely that the study would only have detected very large effects.
The Centre for Pesticide Suicide Prevention (CPSP) have received $8millon from Open Philanthropy. They focus on advocacy for pesticide bans, plus help with finding safer substitute pesticides and with enforcement of new bans. They argue that they have been instrumental in a number of bans. Although they have a team of 20 working in four regions, they say they are funding-constrained, and would like to build a larger team that could operate in more countries. Open Philanthropy recently established Global Health Policy as a new program, naming “suicide prevention through means restriction” as one of the four focus areas. This suggests to us that funding may become easier to acquire in the space, and additional philanthropic funding may become less impactful.
We think that pesticide suicides have probably peaked and begun to decline globally. India and China accounted for most pesticide suicides globally and have seen large declines in recent decades. Targeting smaller countries is likely to be less cost-effective, and yet may be an extremely powerful intervention. It is not clear whether CPSP would use extra funds efficiently: they “are guided by the human rights-based approach” and make no explicit commitment to maximizing the good they do.
It may be possible for other organizations to complement the work of CPSP. Ideas include:
- Helping governments with enforcement[6] of pesticide bans
- Identifying countries with a pesticide suicide problem. Record-keeping is notoriously bad in many African countries, where suicide is taboo and often criminalized. CPSP often cross-reference police, hospital and survey data in an effort to estimate true rates
Our BOTEC attempts to account for the fact that much of the most important advocacy has been done or is being done, and we are highly uncertain about the marginal value of extra work in this space. We attempt to account for this by examining the effect of advocating a small country (population 10 million), as these are less likely to have already been targeted, and assuming a relatively low baseline rate of pesticide suicides (as may be expected from a country that has already banned some pesticides). We estimate that the expected cost-effectiveness of pesticide restriction advocacy has an 8% chance of exceeding GiveWell top charities’ cost-effectiveness. It seems plausible that advocacy in a well-chosen target country could outperform GiveWell top charities.
Type | Intervention | Cost-effectiveness compared to cash transfers[2] | Proportion of benefits from mental health |
Suicide prevention | Pesticide ban advocacy | 7x | 100% |
Lithium supplements
Summary:
- Lithium is widely prescribed as a mood stabilizer and is associated with lower rates of suicide
- There is evidence that populations with naturally-occurring lithium in their drinking water have lower suicide rates
- If successful, policy advocacy for adding lithium to the water supply could cut suicide rates across the population
- There are a number of positive/negative effects that are difficult to predict
Lithium is well-known as a mood stabilizer that is widely prescribed for Bipolar disorder, and is associated with lower rates of suicide. A meta analysis by Cipriani et al. in 2013 found that patients given lithium had significantly lower rates of suicide than those given a placebo (odds ratio 0.13, 95% confidence interval 0.03 to 0.66). Lithium treatment comes with the risk of damage to the thyroid gland and the kidneys, and patients must have their serum lithium levels monitored in order to minimize the danger (Young & Hammond, 2007).
A number of studies have explored the link between levels of naturally-occurring lithium in drinking water and suicide rates in the population. These levels of lithium exposure are far lower than among those taking lithium medication, and it is unknown whether lithium has a physiological effect at such low doses.
Generally there seems to be a trend that areas with “high enough” lithium levels often do display significantly lower suicide rates. Knudsen et al. (2017), a 22-year study in Denmark, where lithium levels range from 0.6 to 30.7 μg/L, found “no significant indication of an association” between lithium and reduced suicide rates. However, they point out that “[p]revious studies that found a significant association with suicide consistently reported the highest lithium exposure levels with up to 59 µg/L in the Oita prefecture in Japan [16], 121 µg/L in Greece [13], and 219 µg/L in Texas [7]. Conversely, studies with the lowest levels up to a maximum of 12.9 µg/L in the Aomori prefecture in Japan [6] and 21 µg/L in the east of England [15] did not find an association, like in our present study in Denmark.”
The two existing meta-analyses on the subject find that lithium in drinking water reduced suicide risk. Barjasteh-Askari et al. (2020) find an odds ratio of 0.42 (95% CI: 0.27 to 0.67; p-value <0.01), while Memom et al. (2020) get a pooled β = −0.27 (95% CI −0.47 to −0.08; P = 0.006, I2 = 83.3%). Both studies found a stronger effect among males. It should be noted that all studies apart from Knudsen et al. (2017) rely on regional suicide rates and therefore fail to account for individual exposure to lithium and for underlying differences between populations.
Psychiatrist Dr Moosajee Bhamjee openly called for lithium to be added to Irish drinking water in 2011, but no country has yet begun to do so. On the release of Memom et al. (2020), Professor Anjum Memom suggested that “[n]ext steps might include testing [the] hypothesis by randomised community trials of lithium supplementation of the water supply, particularly in communities (or settings) with demonstrated high prevalence of mental health conditions, violent criminal behaviour, chronic substance abuse and risk of suicide. This may provide further evidence to support the hypothesis that lithium could be used at the community level to reduce or combat the risk of these conditions.”
Araya et al. (2022) assesses the feasibility of introducing a policy to add lithium to drinking water to decrease suicide risk. They provide an excellent summary of pros and cons, including the possible negative effects of increased suspicion about government motives (as we have seen with the water floridation “controversy”) and increased use of bottled water.
Our opinion is that regional trials could provide evidence that may motivate future country-level interventions to add lithium to the water supply. It would be best to trial this in a country with high trust in the government to minimize downside risks. The relative rarity of suicide and the possible slow-acting effects of low-level lithium means that such trials would take years to gather results.
This is the most speculative intervention we evaluate, so any calculations should be interpreted accordingly. Our BOTEC finds that advocating for a small country to pilot lithium supplementation could have large benefits. The expected benefits increase further when we consider that promising experimental results may prompt other countries to begin supplementing their water supplies with lithium. We estimate that the expected cost-effectiveness exceeds GiveWell top charities in 40% of cases.
Type | Intervention | Cost-effectiveness compared to cash transfers[2] | Proportion of benefits from mental health |
Suicide prevention | Lithium supplementation study | 38x | 100% |
Attitudes to suicide
Many LMICs have no strategies for preventing suicide. Although the benefits would be hard to predict, it seems highly likely that “helping” governments to strategize could be highly impactful:
- Decriminalizing suicide would make it much easier for suicidal people to seek help
- Centralized record-keeping would illustrate the scale of the problem and would provide a gauge of the effects of suicide-reduction efforts
- Countries with a suicide reduction strategy would be more likely to endorse restrictions on deadly pesticides and other means of suicide.
Critical research gaps
- The direct mental health effects of tackling risk factors. Too much of our understanding is correlational, and we may be overestimating the effects that tackling risk factors would have. It would be good to have RCTs that evaluate the mental health impact of interventions which target physical health, or to simply start including mental health metrics among the variables measured in future poverty and physical health work
- The effect of mother/child educational interventions on mental health in adolescence and adulthood (most studies only measure change in knowledge and attitudes, and have short follow-ups (see Klasen & Crombag, 2013). This would require studies spanning many years, which are expensive and difficult to conduct.
Conclusion
Mental illness is clearly linked with adversity in childhood, poor physical health, and being the victim of abuse. These correlations can be valuable for targeting groups who are more likely to be present or future sufferers. Especially with children, risk factors can help us help people before mental illness manifests. However, preventative interventions will always be hits-based: some efforts will be spent on people who were never going to suffer mental illness.
There is an implicit assumption that preventative interventions targeting mothers and children have an edge over those that target adult sufferers. In the absence of long-term studies that track the impact of early-life interventions, we are unable to endorse this assumption.
It would certainly help to diagnose mental illness sooner. But we suspect that truly preventative interventions are best when they are cheap and scalable. For example: policy changes that encourage healthy lifestyles, or new laws that restrict access to deadly means of suicide.
We often don’t know how much of the correlation between risk factors and mental health is driven by genetics or other hidden variables. In order to understand which “nudges” best promote mental health, we need long-term studies to evaluate the counterfactual impact of tackling risk factors.
Intervention BOTECs
[Link to full distributional model]
Here we provide estimates of the cost-effectiveness of various mental health interventions. These should be considered as preliminary “best guesses”, as most of the inputs are either subjective estimates or are taken from others’ analyses.
- We estimate the costs of a hypothetical intervention, and generally assume that it is well-run and operating at scale.
- We discount costs borne by governments, on the basis that these funds are redirected from other types of government expenditure that are relatively inefficient
- We give cost-effectiveness in terms of DALYs. For psychotherapy and child poverty grant advocacy, we had to convert the effect size from measures of mental health into DALYs, which introduces considerable uncertainty
- As always, users should consider how their moral standpoint affects these results, especially when comparing mental health interventions against GiveWell top charities.
How it works
This spreadsheet model is put through UseCarlo.com, which performs a Monte Carlo simulation on Carlo with 1500 runs. Each input (eg. the effect size of an intervention, or the cost per person treated by an intervention) is modeled as a random variable. For each run, the model takes a sample of each random variable and computes the corresponding cost-effectiveness. These 1500 cost-effectiveness estimates can be used to understand the uncertainty in the results. To adapt the model, simply make a copy of the spreadsheet, change the inputs, then re-run the simulation. The outputs used to produce the table below are available in spreadsheet form here.
The next page provides a summary of the results. After that is an analysis of the key trends.
The figures below are mostly derived from subjective estimates and should be used as a guide only!
See the next page for an explanation of each column.
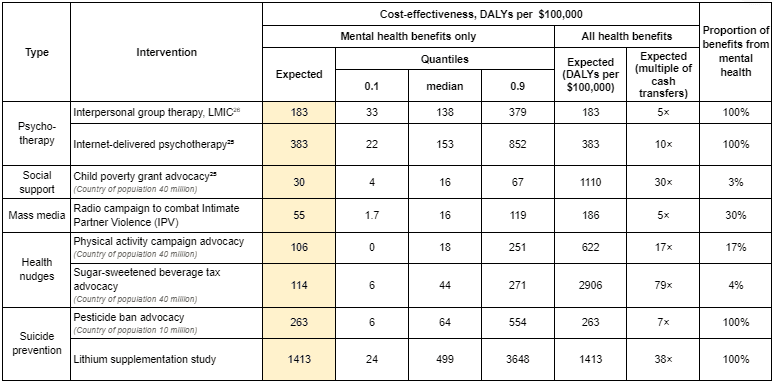
How to read the table:
- We model the expected ex-ante cost-effectiveness of each intervention. This means we are estimating the average cost-effectiveness of a future action. For example, the ex-ante cost-effectiveness of a game of roulette is $0.97 per $1 invested, while the ex-post cost effectiveness can only be $0 or $36 per $1 invested. It should be noted that some of the interventions in the table above (those that depend upon binary policy decisions) are likely to have an ex-post cost-effectiveness of zero.
- Mean cost-effectiveness is the mean of all cost-effectiveness outputs. The Median cost-effectiveness is the middle value among the outputs. 10% of outputs are lower than the 0.1 quantile, and 90% of outputs are lower than the 0.9 quantile.
- According to our estimates, the average cost-effectiveness among GiveWell top charities is 737 DALYs per $100,000.
- Mean (multiple of GW top charity) simply expresses the mean cost-effectiveness as a multiple of our GW estimate.
- Probability of exceeding GW top charity gives the proportion of Monte Carlo outputs that exceed 737 DALYs per $100,000. We are not certain what probability counts as “good”, but we would point out that GiveWell top charities are themselves uncertain, and that we would expect most of them to score well below 50% on this metric.
Analysis
- Mean cost-effectiveness is driven by a minority of highly cost-effective possible scenarios. Mental health interventions are uncertain, so funders should be discerning when considering grant applications. Even for promising-looking proposals there will be a high degree of uncertainty, so funders should be willing to take a “hits-based” approach.
- Cost is critical. For all interventions, cost was among the most important variables. Reducing cost is critical for building a better intervention, and reducing uncertainty about costs is key to making better funding decisions.
- Favorable conditions are required in order for interventions to rival GiveWell top charities. Reducing the cost of interventions is critical for direct work. For policy interventions, working with the most tractable governments and/or the largest countries will boost the expected cost-effectiveness considerably. Lithium supplementation seems to be highly promising, but it is the least-understood intervention on the list.
- Policy interventions hinge on the likelihood of advocacy success. This is a very difficult thing to measure. We estimate that the probability of success is 11% (90% confidence interval: (1%,30%)) for all policy interventions. Opportunities that are more promising than this should be valued more highly. In reality, successful lithium supplementation advocacy (for which there is no historical precedent) is probably less likely than successful SSB tax advocacy.
- The best mental health interventions may not directly target mental illness. Health “nudge” policies may be so powerful that their net effects on mental health are greater than targeted interventions.
- ^
This is probably due to regression to the mean, since participants are screened for serious illness, and may also be caused by response bias and placebo effect.
- ^
This is based on CEARCH’s analysis of GiveWell-recommended charities, which estimates that donations to GiveDirectly avert 37 DALYs per $100,000. This implies that the average GiveWell top charity is approximately 20× cash.
- ^
For illustration, a 2022 meta-analysis by Bello et al. found a staggering 48% prevalence of depression in Africa. It relied entirely on studies that used survey data.
- ^
Although suicide record-keeping has been, and continues to be, poor across much of the world
- ^
The reader should be aware that the increase and decrease of the suicide rate also coincides with the beginning and end of the Sri Lanka civil war. Aida et al. found that suicide rates were not higher in the districts most affected by war, suggesting that the war does not account for the rise and fall of the national suicide rate.
- ^
Poor enforcement can undermine the effectiveness of a ban. In Nepal, which has a porous border with India, methyl-parathion was found to be the most common pesticide used for suicide despite having been banned years earlier.

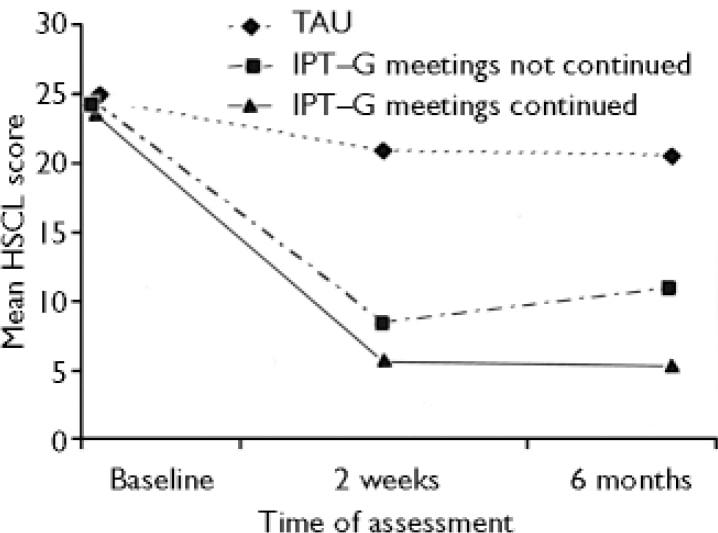
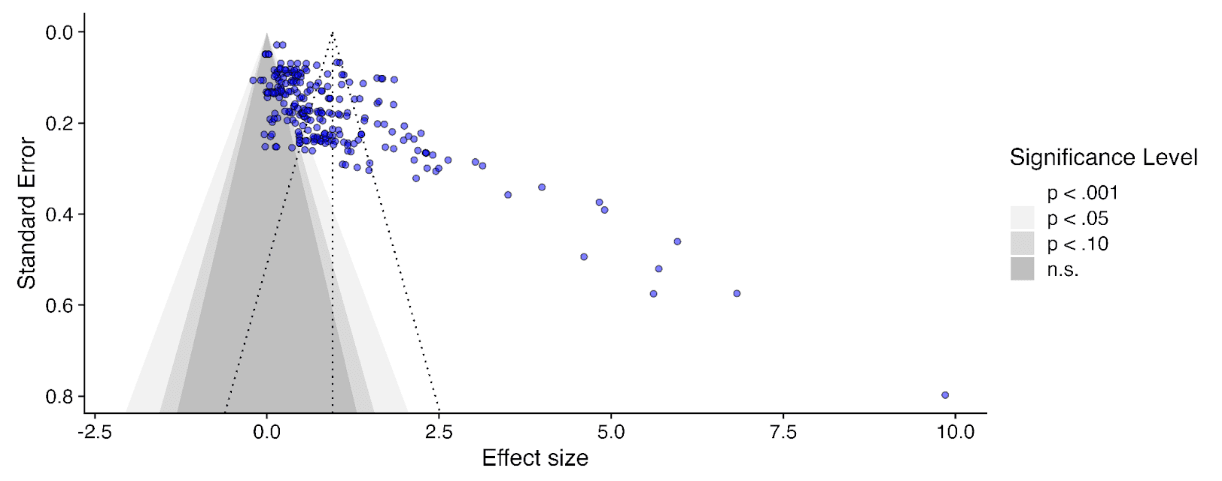
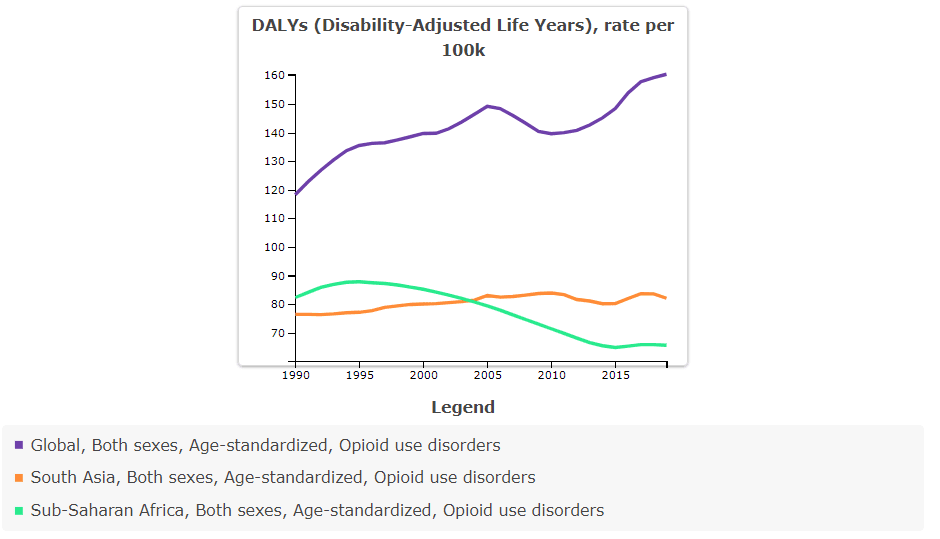
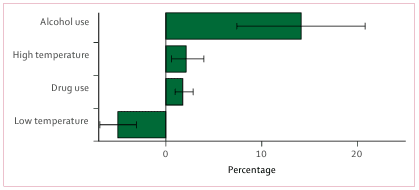
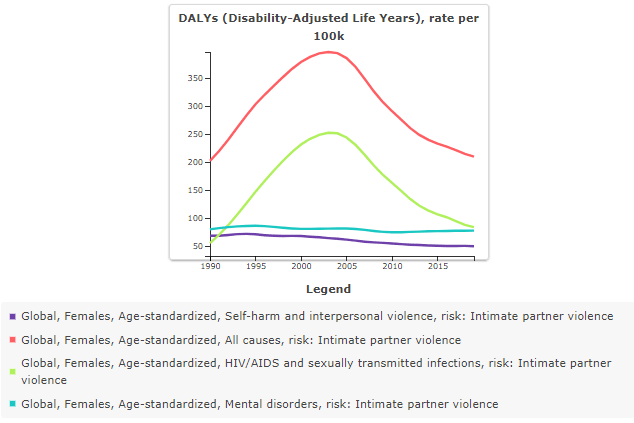
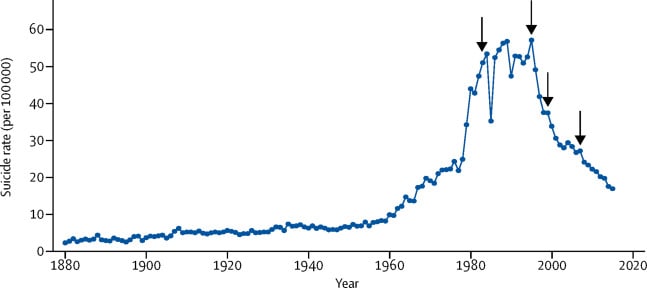
I love the clear way you write here, and the incredibly wide range of interventions you have considered. I think this is a really important summary you've put together, and I'm surprised it's not far more upvoted, maybe it will happen! This is a great place for those interested in cost effective mental health reduction to start, and a credit to CEARCH.
I think alcohol reduction and pain relief are quite underexplored and have potential.
I might comment more later, I had one query about this statement I didn't quite understand "In theory, a well-conducted RCT would experience equal amounts of response bias in its control and intervention group".
Why would this be the case if the participants are not blinded, which they can't be here. If you know your are are not getting the intervention I would have thought you might be more inclined to respond with lower scores under all 3 bias types you discussed, and with the intervention give higher scores. I might be missing something but I'm not sure why we would expect the bias to move the control and intervention group in the same direction.
Nice one!
Thank you for the kind words, Nick!
Completely agree that if the participants know they are receiving a special treatment they are likely to show more response bias. By "well-conducted RCT" I was thinking of studies with an active control like Nakimuli-Mpungu et al. (2020) in which patients "were randomly assigned to deliver either [group support psychotherapy] or group HIV education". If done well, the participants won't know which treatment the scientists "want" to perform better and so response bias will be constant.
Gotcha makes sense. That's very true love the active control!
Great report, Stan! I've subscribed to follow your posts. I appreciate you collating all the evidence and conclusions of the data in the mental health space.
Regarding alcoholism, I'm a fan of Johann Hari's conclusion that "the opposite of addiction is [positive human] connection." Stanford research supports this with their meta-analysis of alcohol treatment programs, finding the peer-support system in 12-step programs to be most effective.