TLDR
- Who we are: Vida Plena (meaning a ‘flourishing life’ in Spanish), which launched in 2022 via Ambitious Impact/ Charity Entrepreneurship.
- What We Do: Combat depression and anxiety by fostering hope and connection through community-based group therapy sessions.
- Why We Do It: Because untreated depression drives immense suffering, yet remains one of the most neglected health burdens in low-resource settings.
- Where We Work: Ecuador, with plans for regional expansion starting in 2028
- Results: 84% of participants improve clinically in depression and anxiety. 82% had reduced suicidal thoughts.
- Funding Gap: Total of $175,000.
- $54,000 will allow us to expand to Manta, a coastal city plagued by gang violence, the Indigenous Amazon in Tena, and Puyo.
- Why Now? Nationwide expansion is within sight. We’re getting governmental buy-in, reducing our costs of operation, and we’re demonstrating that our model works within various cultural contexts throughout Ecuador.
Before reading on, how strongly do you think mental health improvements reduce total human suffering? Please share your reasoning in the comments.
Context for Our Work
Depression is one of the largest drivers of disability worldwide, yet remains chronically neglected in global health. Given that globally, mental disorders account for about 5.4% of all DALYs (Our World in Data), while malaria accounts for ~2.5% (Our World in Data), mental health’s burden rivals this of well-known physical diseases. Suicide alone claims more than 720,000 lives annually (WHO), a toll comparable to malaria’s ~597,000 (WHO).
In Ecuador, mental health represents a profound but neglected burden. In Ecuador, 43% of the population has experienced depression or anxiety in their lifetime (Our World in Data), placing the country among the ten worst worldwide (Gallup). Depressive disorders account for about 9 percent of Ecuador’s total years lived with disability, per WHO-referenced estimates cited in recent national analyses (Journal of Affective Disorders).
Despite this burden, only 2.3% of Ecuador’s national health budget is spent on mental health (Ministry of Public Health); however, “The majority of this budget is allocated to the only psychiatric hospital and the purchase of services in private specialized mental health facilities” (Ministry of Public Health). The result is near-total inaccessibility for rural and low-income communities.
This crisis is further neglected in terms of philanthropic funding prioritization. Despite 41% of rural Ecuadorians living in poverty (Applied Research in Quality of Life) and coastal Ecuador facing some of the highest violence rates worldwide (The Economist), Latin America attracts only about 9% of global philanthropic resources (OECD), compared to 61% directed to sub-Saharan Africa.
The impact of untreated depression extends beyond personal suffering; it significantly reduces educational achievements, lowers employment rates, deteriorates physical health, and shortens life expectancy. The economic toll of this is enormous: untreated mental health in the Andean region results in the loss of an estimated 5% of GDP (The Lancet).

What is the evidence base for the intervention you are employing?
Vida Plena’s core intervention, group interpersonal psychotherapy (g-IPT), is supported by strong evidence and rigorous quality standards. The World Health Organization recommends g-IPT as a first-line treatment (WHO).
Vida Plena is the first organization in Latin America to implement g-IPT.
The effectiveness of interpersonal therapy has been demonstrated in a meta-analysis collating 12 studies (American Journal of Psychiatry), which notably concludes, “There is no doubt that IPT efficaciously treats depression, both as an independent treatment and in combination with pharmacotherapy. IPT deserves its place in treatment guidelines as one of the most empirically validated treatments for depression.”
Foundational studies further bolster the efficacy of g-IPT. Bolton et al. (2003) demonstrated its impact in Uganda, showing a mean reduction of 17.47 points in depressive severity among g-IPT participants, compared to only 3.55 points in the control groups. Similarly, Bhat (2022) showed that brief 6–8 session therapies by community counselors produced lasting benefits, leaving participants 11 points less likely to be depressed years later, further validating Vida Plena’s model.
Vida Plena is trained by and pursuing certification through Columbia University’s Global Mental Health Lab, and is one of the few community organizations to be selected for training by the WHO in their EQUIP methodology to ensure service quality. As the first organization in Latin America on the path to be certified as trainers of trainers for g-IPT, Vida Plena is committed to scaling proven mental health solutions with exceptional fidelity.
Track Record so Far
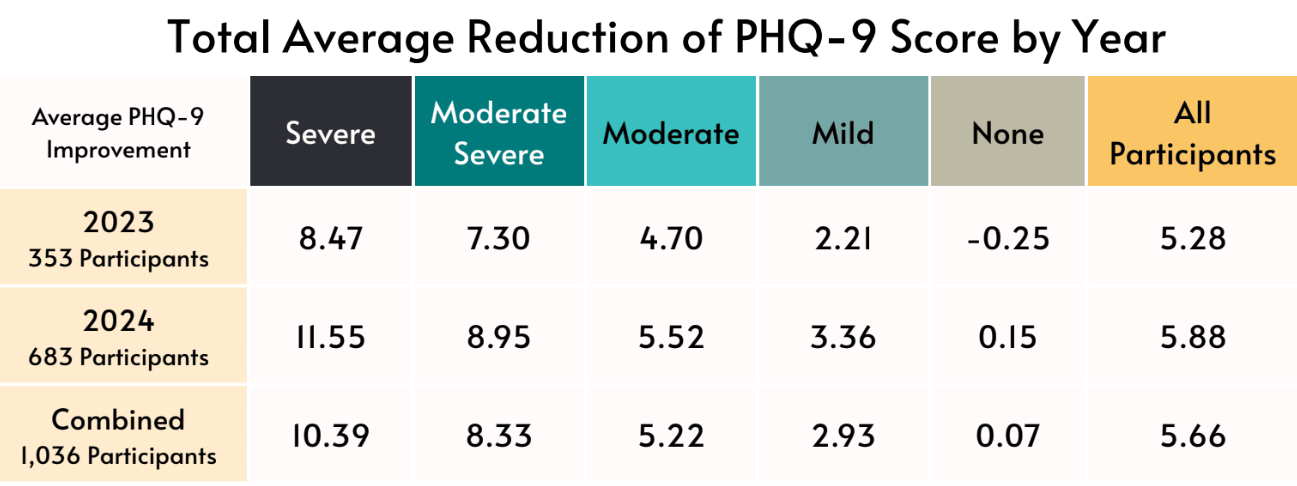
Vida Plena’s strategy has followed a deliberate trajectory. In 2022, we piloted direct service delivery with an internal team of facilitators to build the operational experience and evidence base needed for scale. Since then, from 2023 - 2024, we directly served nearly 1,500 participants, with another 1,000 projected by the end of 2025.
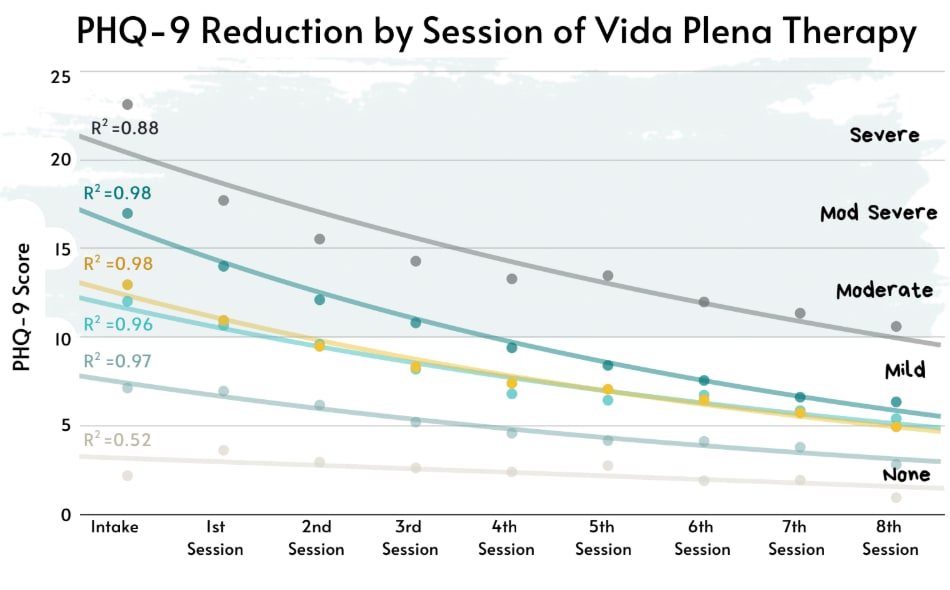
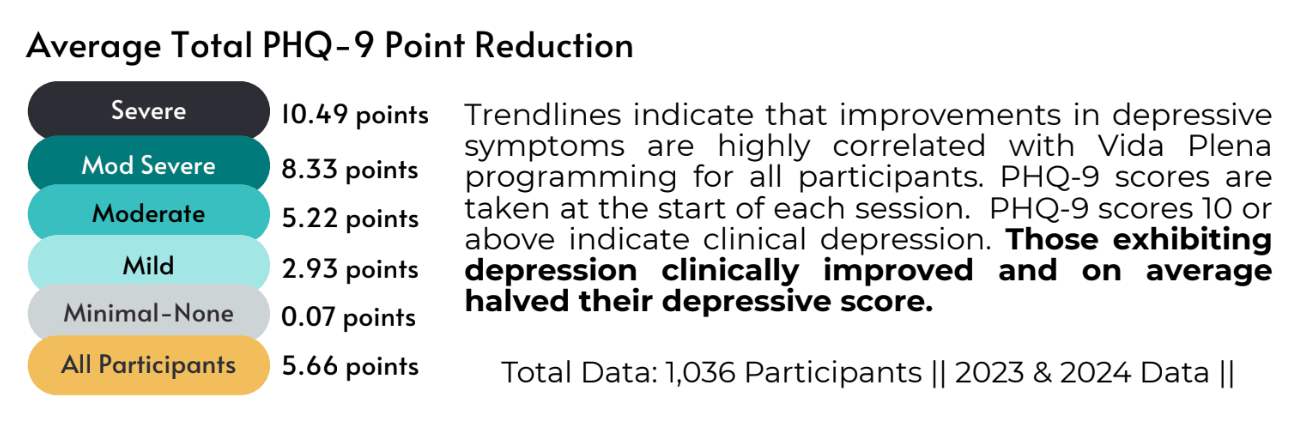
Outcomes are consistently strong:
- 84% of participants showed clinical improvement on depression and/or anxiety
- 82% reported fewer suicidal thoughts
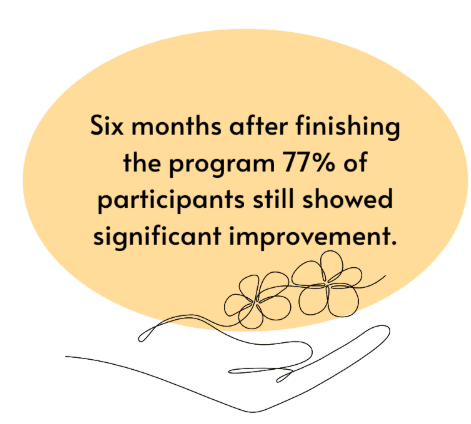
These results far exceed the reported spontaneous remission rate of 12.5% (Journal of Affective Disorders), and improvements are sustained at three- and six-month follow-ups.
Read more in our 2024 Impact Report.
Now Entering Phase 2: Scaling Through Government Systems
Vida Plena is transitioning from direct service to government-led delivery, utilizing our team to train, supervise, and ensure fidelity.
Quito (Municipal Level):
- Trained 9 staff in 2024 (pilot report)
- Outcomes were strong enough that the Health Department requested rapid expansion
- Trained 24 more staff in early 2025, plus a second city agency joined voluntarily
- Government teams now deliver care under Vida Plena supervision and shared monitoring
Imbabura (Provincial Level):
- Invited by the provincial government to train 15 gender-based violence advocates
- First adoption of our model at the provincial scale
Why this is compelling:
- Governments are not just agreeing—they are asking us to expand
- Public staff, existing infrastructure, and local budgets create a high-leverage path to national scale
- Vida Plena provides the expertise and quality control; governments provide the workforce and reach
This positions Vida Plena to embed evidence-based mental health care directly into Ecuador’s public system.

What’s Next
Vida Plena stands at a pivotal moment in its mission to strengthen and sustain transformative mental health interventions in Ecuador. Having successfully partnered with the City of Quito and the Province of Imbabura to embed our evidence-based model within government systems, we are now ready to extend this work further.
By 2026, our goals are to:
- Train three additional provincial government teams, equipping 45 staff to deliver high-quality group therapy to ~900 people annually.
- Maintain and grow our direct service operations, reaching ~1,200 participants while continuing to generate evidence and test program innovations.
- Strengthen and scale our existing government partnerships, enabling ~500 participants to be reached annually through municipal and provincial teams.
- Build long-term sustainability by training new supervisors, including preparing government agencies to develop their own supervisory capacity.
The big vision is national adoption. With strong evidence, established government partnerships, and a key champion now positioned in the Ministry of Health, Vida Plena is creating the systems and political momentum needed for Ecuador to deliver mental health care at scale.
Cost effectiveness
- Delivery strategy:
- Direct service supports ongoing testing and model refinement
- Municipal partnerships drive all meaningful scale at lower marginal cost
- Projected reach for 2026: ~2,600 people
- 1,400 through municipal and provincial partners ($82 per person)
- 1,200 through direct service ($192 per person)
- Average cost per participant: $112
- Comparison to private therapy:
- Private therapy in Ecuador costs $40/hour
- Vida Plena provides 14 hours of structured support
- Equivalent private-market value: ~$560 per person
- External cost-effectiveness estimates (Bloom, based on 2024 data):
- Impact per participant estimated at 1.16 to 1.70 WELLBYs
- Estimated cost-effectiveness: 4.98 to 22.70 WELLBYs per $1,000 donated
- This corresponds to 0.66 to 3× the cost-effectiveness of GiveDirectly
- Vida Plena’s 2025 cost reductions mean future estimates may be more favorable than those modeled using 2024 data.

How marginal funding accelerates our work
While our overall funding need for 2026 is $175,000, marginal contributions can unlock key pieces of our next phase of growth. This funding will serve as a catalytic investment, delivering concrete impact in 2026 while laying the groundwork for long-term, systemic change nationwide.
$18,000 will allow us to launch our program in a new municipality, expanding access to mental health care for approximately 800 people per site. We plan to reach three new municipalities next year, and each contribution of $18,000 fully unlocks one additional expansion.
$23,000 will fully fund our Monitoring, Evaluation, and Learning Coordinator, a role that is essential for preparing our upcoming RCT and improving our internal analytics. This investment strengthens our ability to generate high-quality evidence, refine our model, and continue improving participant outcomes.
$15,000 will support the development and rollout of our supervisor training program, which is key to scaling with quality. Strengthening local supervisory capacity allows us to maintain fidelity as we grow and ensures that rural and Indigenous facilitators receive the mentorship they need.
Each of these steps compounds our ability to expand responsibly, deepen our research agenda, and reach thousands more people with accessible and culturally rooted mental health support. The end goal is to build a scalable, evidence-driven care model that can serve as a new standard for community-based mental health in low-resource settings.
How You Can Help
Donate:
- If you'd like to support us, consider donating on our website. Donations are tax-deductible for US residents. For bigger contributions, let's chat! Drop an email to joy@vidaplena.global
Stay in Touch:
- Want to keep up with our work? Follow us on LinkedIn, Instagram, or subscribe to our newsletter.
Tell a Friend:
- Know someone who'd be interested? Share our story! Whether it's this post, our website link, or encouraging them to join our newsletter, your recommendation matters.
Thanks for being part of our journey!



I'm planning to donate ~5-10% of my giving this year to Vida Plena, and I thought it might be worthwhile to explain why ahead of the Donation Election.
I find it unlikely that directly paying the costs of g-IPT is sufficiently cost-effective given other potential uses of EA-sourced funds. So for me, the critical question for me is whether Vida Plena can attract sufficient government and/or non-EA private interest to cover most costs in time (probably with an assist from a reduction in costs due to economies of scale).
I'm encouraged by the progress in working with government entities, and see the engagement from Columbia and the WHO as a loose proxy for potential attractiveness to non-EA private donors. Moreover, I think it's plausible that Vida Plena is at a "pivotal moment" as the post says, and that timing suggests that giving this year could be more impactful then most years.
So this is my less-certain but higher-potential-upside global health donation for the year.
HI Jason,
Thank you so much for both the donation and for publicly sharing your reasoning. I really appreciate you taking the extra step to make this visible; that kind of transparency is genuinely valuable to the community and to us.
I share your core framing almost exactly. The long-run case here really does hinge on whether government and large institutional funding materializes, and that is a real bet with meaningful risk. Support from the Columbia team and the WHO is encouraging but far from a guarantee, and I want to be very open about that uncertainty. At the same time, even if the big bet on government funding doesn’t work out, the harm is limited and mostly turns into learning. But if it does work, the upside could be very large. If it succeeds, it unlocks a scale that EA funding alone could never sustain.
I also strongly agree with your point about timing. Marginal funding this year is especially leveraged toward evidence, partnerships, and proof of viability. That makes support at this moment unusually impactful relative to most years.
Thank you again for your support and for articulating this so clearly. It truly means a lot at this stage.
Currently depression is the number one health disability globally and on track to be the number one killer in the near future, killing more than cancer, heart attacks, hunger, etc. Now is the time to get ahead of it. Also diminishment of individuals and their communities and productivity on the path to death. For example, a depressed mother stops taking care of her family well…if they have to walk miles to take the kids to a health clinic, now that doesn’t happen and the children’s health goes down. Many of us weren’t paying attention as depression grew to now rival the top human killers.
Thanks so much for this, Jeffrey. You’re absolutely right about the far-reaching spillover effects of depression on families, communities, and long-term health and productivity. And though they can be hard to measure, these impacts are still incredibly real. Anyone who has experienced depression personally, or through a loved one, knows just how deeply it affects the people around them in ways that often go unseen. Really appreciate you naming this broader reality.
Good luck!
Thank you so much for the encouragement and support, Joey!