[This is my first EA Forum post so any comments/reviews on how this could have been more useful are welcome. This was written for the EA Cause Exploration Prize contest ]
Epistemic status (how confident I am) -
Slightly confident.
The literature on anemia, the role of iron in health and disease, and fortification as an intervention turned out to be far more vast and nuanced than I had estimated. The key point upon which the advantages of targeted interventions over mass supplementation/fortification relies on is the association between increased iron levels and diabetes/hypertension, which comes from a pre-print paper not subject to peer-review. However, the authors of the paper are well-reputed with their previous work being relied on GiveWell and their data is based on a large comprehensive survey.
I also realized doing half-decent cost-effectiveness calculations would take a lot more time to learn to do well and I could not really perform any. This means that any conclusions I present are reliant more on intuitive ~this-simply-makes-sense~ than hard numbers.
Main Takeaways
- Anemia, iron-deficiency caused or otherwise, is a significant source of DALYs in India. While current interventions of mass iron supplementation and iron fortification are widely pursued by the government and private players, including GiveWell supported organization, these interventions may be less effective and more harmful than previous analyses suggest.
- This is primarily based on new analysis of data from the Comprehensive National Nutrition Survey (CNNS) 2016-18 by HPS Sachdev and colleagues, who most prominently find that providing 10 mg of iron/day by fortification could increase the prevalence of diabetes by 2%-14% across states of India.
- An alternative, more precise method of treating anemia using screen-and-treat strategies can eliminate such risks while also allowing for differential treatment of different types of anemia. Such strategies may cost around $1.4/person for each 6mo cycle of screening-treating.
Current problem and solutions
The current story of anemia in India
Anemia is a condition with a multifactorial etiology characterized by a decrease in red blood cells and reliably marked by a decrease in hemoglobin levels. The loss of red blood cells leads to a deprivation of oxygen with numerous physiological, cognitive and economic implications. Anemia during childhood and adolescence can lead to severe developmental issues, some of which may be irreversible. (WHO)
Anemia is often associated with a deficiency of iron. According to an analysis in Nature’s Scientific Reports based on data from a national 2016 survey, 60% of 112k surveyed children in India were anemic in 2016 and children with anemia were more prone to being iron deficient (odds ratio [OR]: 0.981 (0.961–1.001) (Onyeneho 2019). However, deficiencies in other micronutrients such as the vitamins folate, B12 and A, infections by malarial parasites, worms, and others, inflammation from sub-acute infections, microbiota disturbances as well as hemoglobinopathies (structural defects in RBC’s) are also important factors associated with anemia, many of which have a complex relationship with iron levels. The Institute for Health Metrics and Evaluation estimated iron deficiency to be a leading cause of DALY’s accounting for 10.79 of total DALY’s for adolescents ages 5-14 in South Asia.
Faced with imposing and stubborn anemia prevalences, the Indian government has been providing weekly iron folic acid supplements to government school children since 2012 (Ministry of Health). The Modi government announced a year ago that iron fortified rice would be distributed through various government schemes by 2024.
GiveWell has written a report on iron fortification concluding that “There is strong evidence that iron fortification reduces cases of iron deficiency and anemia” with its current status as ‘actively supporting". GiveWell has also given large grants towards iron supplementation and fortification to Evidence Action and Fortify Health respectively, the latter receiving $8M+ in 2021 to expand wheat fortification in India.
Potential Issues of Current Approach
This piece is motivated by recent evidence that actual anemia prevalence in Indian adolescents may be much lower than previous estimates and that iron supplementation and fortification may be less effective and more harmful than GiveWell analyses suggest. If true, this suggests that targeted anemia treatment, modeled along Test-Treat-Talk (T3) or Screen and Treat (STAR) programs, may be more cost-effective, more robust, and less ethically problematic than current approaches.
Mass iron supplementation and food fortification are broad ‘sledgehammer’ programs that aim to alleviate the burden of anemia by flooding the population with iron. Concerns have been persistently raised that such approaches could lead to adverse outcomes as an excess of iron can give rise to a range of negative outcomes. In particular, attention has been focused on increases in malaria, with the WHO stating iron supplementation should only be carried out in conjunction with malaria prevention strategies in areas with high prevalence and low support. In their report on iron fortification, GiveWell states that their “best guess is that iron supplementation and fortification do not have a meaningful effect on malaria risk” based on a Cochrane 2016 review of malaria and iron supplementation -
GiveWell also notes the potential adverse effect of iron overload, finds little evidence that suggests this could be a problem, and concludes with “we would consider investigating iron overload in more depth if we recommended additional funding to iron fortification programs.” However, in their $8 million grant report to Fortify Health they note that they have not “incorporated any additional evidence on fortification published since that [iron fortification] report.”
This may be an unfortunate lapse because analysis of data from India’s Comprehensive National Nutrition Survey (CNNS) 2016-18 by HPS Sachdev and colleagues, whose work incidentally is “heavily relied on” by GiveWell in their Iron Fortification report, has emerged in the past year that needs to be reckoned with.
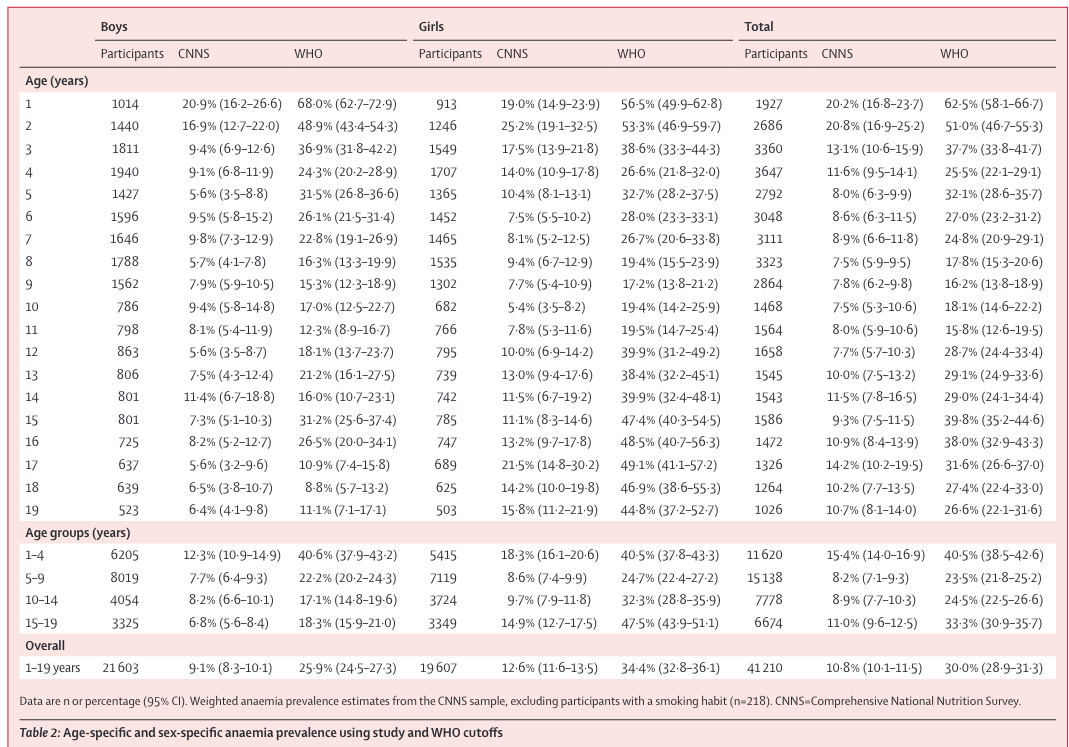
The updates from this work can be broken down into three categories - a) Replacing WHO anemia cutoffs for hemoglobin that are based on non-representative populations with cutoffs based on percentiles from a healthy, representative population results in a 20% drop in anemia prevalence in 0-19 year olds [Lancet, 2021]; b) the current proportion of anemia cases for 5-19 year olds that are due to iron-deficiency is around 20% [J of Nutrition, 2021]; c) the risks associated with increased iron in adolescents can be substantial, mainly associated with a rise in non-communicable diseases (NCDs) [Pre-print, 2021].
The last point about the rise in NCDs is especially worth stressing though it must be noted that the evidence currently comes from a pre-print. Sachdev and colleagues analyzed the same data from CNNS to investigate if serum ferritin levels (a functional form of iron) was associated with high fasting blood sugar levels (FBS - marker of diabetes), high blood pressure (HTN - marker of hypertension) and high total cholesterol levels (TC - marker of dyslipidaemia). They found an “odds ratio (OR) of high FBS, HTN and TC were 1.05 (95% CI 1.01-1.08), 1.02 (95% CI: 1.001-1.03) and 1.04 (95% CI: 1.01-1.06) respectively for every 10μg/L increase in SF. The odds for high TC increased with co-existing prediabetes. The scenario analysis showed that providing 10 mg of iron/day by fortification could increase the prevalence of high FBS by 2%-14% across states of India. Similar increments in HTN and TC can also be expected.”
Why Targeted Treatment - Advantages over broad-level strategies
Compared to sledgehammer programs like mass supplementation and fortification, targeted treatment is like a scalpel that involves screening all adolescents in a school using a complete blood count (CBC), diagnosing specific types of anemia in affected children, and providing tailored treatment and counseling to the child and their parents. Such an approach would suggest significant benefits over mass supplementation and fortification. For one, current approaches tend to be only prophylactic in nature, with severe anemic cases remaining untreated. Two, targeted programs can identify the precise nature of anemia and offer differential treatment for specific anemia etiologies. Three, targeted programs avoid the potential large risks caused by increased iron levels, especially in at-risk populations. This could be especially important in India where a large proportion of children (50%) appear to have at least one biomarker of ‘metabolic obesity’ that predisposes them to diabetes. Finally, the intrinsic need to collect data in such a program offers far more adaptability, responsiveness, and an easier ability to evaluate its effectiveness.
A version of this program was launched by the Indian government in their 2018 Anemia Mukt Bharat, with plans to implement it module wise in Test-Talk-Treat (T3) health camps. However, such T3 camps used digital hemoglobinometers that have been criticized for their poor accuracy as well as not offering the necessary data to allow for differential diagnosis that is afforded by a CBC. Data on the wide-spread implementation and reach of T3 camps remains opaque and likely remains poor, attested by several government schools in Northern Karnataka reporting no such camp ever being held [Insight from fieldwork for Rajalakshmi Children Foundation] This gap in implementation appears readily filled by private players.
A couple of quasi-randomized studies have been carried out on the efficacy of such targeted anemia programmes and appear to have had limited success. (0-6 year olds Dominican Republic, women and children Pakistan) However, these studies have several limitations that prevent strong conclusions. A 2021 protocol for a large cluster RCT that plans to deploy targeted anemia treatment in Telangana, India is available here with data likely to be available soon. It seems fair to assume that if properly implemented, a targeted intervention will have at least the same, if not more, efficacy in treating iron-deficiency anemia as broad-scale iron supplementation, as the method of treatment would be the same and would include the benefits of counselling.
Extremely rough cost estimates
The following numbers are from the Rajalakshmi Children Foundation, a NGO running health and infrastructure development of government schools in Northern Karnataka. [Full disclosure - I am a team member of this organization]
The cost of running a anemia screening health camp at a government school, including equipment, testing, and salaries for all labour necessary, is approximately $1/person. The cost to treat someone with iron or vitamin deficient anemia, including supplements for 6 months and paying a paediatrician, is $4/person. Given a 10% actual anemia prevalence from the new cut-offs suggested by Sachdev and colleagues, the cost of a 6 month cycle of screening-testing would come to $1.4/person. Multiplying this by the number of adolescents in India (250 million), implies a cost of $375 million.
Using Low et al. 2013, a Cochrane Collaboration meta-analysis of the effects of iron supplementation on cognitive development of children aged 5-12 years cited by the GiveWell report, treating anemia leads to an increase in IQ of 4.55 points, among other benefits. I am unsure of how to translate this to economic benefits, this paper suggests a one-point IQ increase translates to 4% increase in welfare growth for the average country. A old 2003 paper by Horon and Ross on the economics of iron deficiency suggests the median total losses of India to iron deficiency in children amount to $15.50 per capita. However, this was based on India having an anemia prevalence of 66% and a GDP per capita of $320. The decreased anemia prevalence using the new hemoglobin cutoffs is 10% and the current GDP per capita is $1900 (2020 estimate). I was unable to calculate the the total GDP per capital loss with this new data using H&R’s method.
Conclusion
I started this piece expecting to find targeted intervention strategies to be more effective in terms of reducing the number of people with anemia but potentially not as cost-effective as mass supplementation or fortification. I expected the latter programs to be undesirable mainly because of their prophylactic nature and the seemingly wasteful nature of simply increasing everyone’s iron levels, irrespective of their anemia status.
However, if the rise in diabetes from increases in iron is indeed true, it seems highly possible that fortification might be actively harmful especially in India. This is something I strong recommended GiveWell and other organizations like Fortify Health to do a deeper dive on.
I also haven’t seen much discussion on the ethically problematic nature of fortification with respect to taking away agency from what people can choose to eat. This is especially true of adolescents in schools who have little option but to eat what their given in government mandated midday meals. I am surprised that this ethical facet was not mentioned anywhere in GiveWell’s reports. From an optics standpoint, if iron fortification does indeed lead to a 2-14% increase in diabetes in adolescents, the decision to give Fortify Health $8M+ can severely damage EA’s reputation. Incidentally, they’re already many pieces in the press on the potential harms of fortification.
This quote from a perspective piece in 2021 by the venerable Sachdev and colleagues is a good way to conclude -
Supplying more by layering multiple nutrient interventions, instead of doing it right, without thoughtful considerations of social, biological, and ethics frameworks could be counterproductive. The cure, then, might well become the malady.
Appendix
[I added this two days after posting this in response to MHR's comment -
References
Is iron status associated with markers of noncommunicable disease in Indian children?- https://assets.researchsquare.com/files/rs-1136688/v1_covered.pdf?c=1638568122
WHO Anemia - https://www.who.int/health-topics/anaemia#tab=tab_1
Determinants of Childhood Anemia in India - Nature Scientific Reports, 2019 - https://www.nature.com/articles/s41598-019-52793-3
Prevalence of Iron Deficiency and its Sociodemographic Patterning in Indian Children and Adolescents: Findings from the Comprehensive National Nutrition Survey 2016–18, The Journal of Nutrition, 2021 - https://academic.oup.com/jn/article/151/8/2422/6287924
Institute of Health Metrics and Evaluation - https://www.healthdata.org/gbd/2019
National Iron Plus Initiative, IJMR 2019 - https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6886130/
Fortification of rice announced by Modi government - https://pib.gov.in/PressReleasePage.aspx?PRID=1814826
GiveWell Iron Fortification report - https://www.givewell.org/international/technical/programs/iron-fortification#Effect_on_iron_deficiency_and_anemia
Fortify Health 2021 Grant report - https://www.givewell.org/research/incubation-grants/Fortify-Health-expansion-December-2021#Cost-effectiveness
Microbiome and Iron - https://academic.oup.com/ajcn/article/106/suppl_6/1688S/4823200
Diarrhea and iron - https://www.bmj.com/content/325/7373/1142.short
Infections and iron - https://www.sciencedirect.com/science/article/pii/S1471490619302571
WHO on iron supplementation - https://apps.who.int/iris/bitstream/handle/10665/204712/9789241549523_eng.pdf
Cochrane review on iron and malaria - https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD006589.pub4/epdf/full
Haemoglobin thresholds to define anaemia in a national sample of healthy children and adolescents aged 1–19 years in India: a population-based study, The Lancet, 2021 - https://www.sciencedirect.com/science/article/pii/S2214109X21000772
Metabolic obesity in Indian children - https://pubmed.ncbi.nlm.nih.gov/33893450/
Anemia Mukt Bharat - https://anemiamuktbharat.info/
‘Screen and Treat for Anaemia Reduction (STAR)’ strategy: study protocol of a cluster randomised trial in rural Telangana, India - BMJ Open, 2021 https://bmjopen.bmj.com/content/11/12/e052238.abstract
Dominican Republic trial - https://academic.oup.com/tropej/article/62/2/116/2375035
Pakistan trial - https://onlinelibrary.wiley.com/doi/10.1111/ajr.12395
Low, 2013, Cochrane 2013 review - https://www.cmaj.ca/content/cmaj/185/17/E791.full.pdf
IQ and Welfare growth - New estimates on the relationship between IQ, economic growth and welfare - https://www.sciencedirect.com/science/article/abs/pii/S016028961630318X
Economics of Iron Deficiency - https://www.smarterfutures.net/wp-content/uploads/2013/12/Economics_of_Iron_Deficiency.pdf
Perspective: When the cure might become the malady: the layering of multiple interventions with mandatory micronutrient fortification of foods in India - The Journal of Nutrition, 2021 - https://academic.oup.com/ajcn/article-abstract/114/4/1261/6329768
The Hindu Press piece - 'Inescapable risks of mandatory iron fortification' by Kurpad and Sachdev - https://www.thehindu.com/sci-tech/science/inescapable-risks-of-mandatory-iron-fortification/article37986787.ece

I appreciate your thoughtfulness and shared goals of addressing anemia in India. Please see my response to critiques of fortification efforts here.
This is really interesting, and something I hadn't thought about before. Doing a quick literature search, there is also previously existing evidence that high levels of dietary iron may impart a diabetes risk. So the effects seen in the paper don't seem crazy, but I did come out of this with a couple of questions/comments.
Thanks for the comment and apologies for the delay in responding!