Marginal Funding Post and Year 2 Updates
Vida Plena in Summary
Vida Plena exists to help people rebuild broken relationships, to grow new connections, and to rekindle hope.
Vida Plena means “Flourishing Life” in Spanish and we strive to help people prosper and regain agency over their lives by providing evidence-based treatment for depression. Vida Plena strives to restore what depression robs; connectedness, professional abilities, and physical health. A 2021 Gallup poll ranked Ecuador as among the unhappiest people in the world, but only 0.04% of the national health budget is spent on mental health care.
As a result, vulnerable Ecuadorians in critical need often lack access to mental health support. Vida Plena aims to address this gap by alleviating depression through accessible, evidence-based group interpersonal therapy (g-IPT), recommended by the WHO. We are the only organization dedicated to scaling mental health care across Ecuador, using a community-based approach that ensures compassionate and culturally sensitive support.

Depression: harming all areas of life
Within every person exists a sense of potential—a vision of what life could be. Yet for too many, challenging traumatic experiences, tragedies, and internal pain obscure this hope, pushing individuals into a spiral of depression and despair.
What drives depression? While its causes are complex, it is frequently triggered by profound disruptions migrating and losing family ties, losing a job, or losing a child. These are community problems that need to be solved in community. These issues extend beyond the individual; they are community challenges that demand community solutions. Research now demonstrates that isolation not only affects mental health but also deteriorates physical health leading to higher mortality. Depression's impact doesn’t stay contained within one individual; it ripples outward, affecting families, friends, coworkers, and the broader community, influencing society at every level.
Depression acts as a force that disrupts our most valued connections, driving wedges between friends, parents and children, spouses, and even leading people to feel cut off and alone. At its worst, depression robs individuals of hope entirely, leaving them so disconnected and desolate that suicide may seem like the only escape.
It Takes a Village - What We’re Asking For
1. Help a Life Flourish
$233 Sponsor Someone Through the Program
- You can save a life as depression not only causes immense human suffering but is a deadly disease. Approximately 24% of the individuals we support are at high risk of suicide and as a result, face a 3- to 11-fold increased likelihood of dying by suicide within the next 30 days.
- Even those who struggle day by day fighting the endless void of hopelessness are at risk of social isolation, falling into abusive relationships, substance abuse, unemployment, and loss of personal agency.
- Here are just some of the scenarios in which Vida Plena helped people in 2023:
- Escaping Domestic Violence & Emotional Abuse
- Several mothers got themselves and their children out of physically abusive relationships.
- Several women escaped cycles of emotional abuse and infidelity that destabilized the home and affected their children.
- Building Emotional Intelligence and Resilience
- One woman emotionally recovered after being kidnapped, physically assaulted, and sexually abused. She built up her support network, gained newfound confidence and self-esteem, and eventually rekindled her small business branching out to newfound markets.
- Mothers learned emotional resilience and repaired relationships between themselves and their children, rekindling and fostering an environment of trust and love.
- Daughters learned how to reestablish relationships with healthy boundaries with verbally abusive parents.
- Escaping Domestic Violence & Emotional Abuse
- Here’s what some people who have gone through the program say:
- “I was a drenched and freezing chick. Vida Plena was the hand that pulled me in from the dark, with the invitation to sit around a warm fire. Around that ire were other women singing, they were singing songs of hope. And as Vida Plena tended that fire, I rediscovered my strength.”
- “Now I know that I have similar problems to those of my friends in my group. Somehow this made me think that it’s possible to rise above them. Helping others overcome their problems gives me a new perspective on my ability to resolve and face challenges.”
If you’d like to sponsor a flourishing life, you can donate here.
2. Funding for a Group Facilitator
$800 Monthly / $9,600 Annually
- Vida Plena employs a system of community facilitators to conduct the group sessions. Each facilitator is responsible for up to eight groups and routine follow-ups. Our facilitators are paid staff, not volunteers, enabling us to support not only individuals struggling with depression but also the community members and families who make this program possible.
- We also employ supervising psychologists to assist the facilitators, provide support, and make recommendations if a participant needs specialized care beyond the scope of Vida Plena.
3. Funds to Expand
$50,000
- Our goal is to reach 2,000 people by the end of 2025. With our newly forged governmental partnerships with the Secretaria de Salud and Prefectura de Imbabura implementing our model, we’ll be able to reach rural communities outside our previous network. We currently have programs in Quito (the capital) and Otavalo (a Kichwa community) but we would like to further expand from these areas targeting more rural and disadvantaged populations outside of the major cities.
Expansion requires us to scout for new potential facilitators, conduct interviews, train them, and run outreach programs to let people in the area know of our services.
the Vida Plena Quito-based team
Hope: The Catalyst for Change
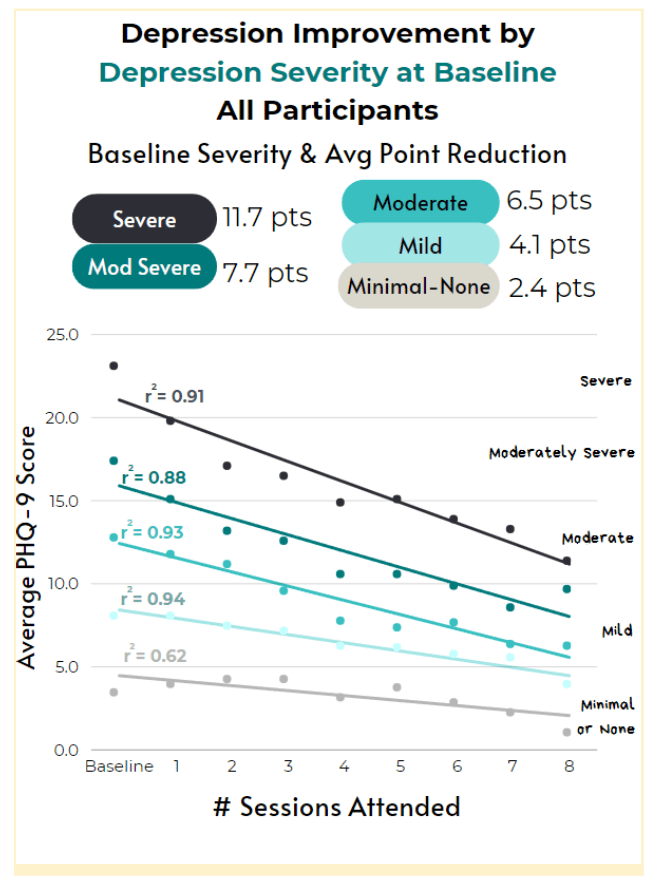
Vida Plena delivers group interpersonal therapy (g-IPT), an evidence-based approach recommended by the WHO as a first-line treatment for depression. The program consists of eight weekly sessions, conducted in person or virtually, with groups of no more than eight participants. Having first been proven effective in other LMICs, g-IPT has also demonstrated long-term positive effects. We have adopted this model in Ecuador to strengthen community bonds, build supportive networks, enhance emotional resilience, boost self-esteem, instill hope, and equip participants with coping skills to face future challenges.
Vida Plena trains local community members to facilitate g-IPT sessions, ensuring that change arises from within, led by individuals who understand the cultural nuances and unique daily challenges of their communities—whether rural, urban, or indigenous. This approach is crucial, as 90% of our participants come from vulnerable populations in Ecuador, including those facing food insecurity, refugees, migrants, Indigenous people, incarcerated women, female heads of households, and the elderly. Each group faces distinct challenges that require culturally informed, empathetic care.

In 2022 we launched our pilot program with 50 participants and in 2023 scaled nearly nine times and by the end of 2024 we will have treated a cumulative total of 1,200 participants. The average participant lives in an average family household of four who all receive the benefit of a healthy family member leaving our impact more widespread than just direct participants.
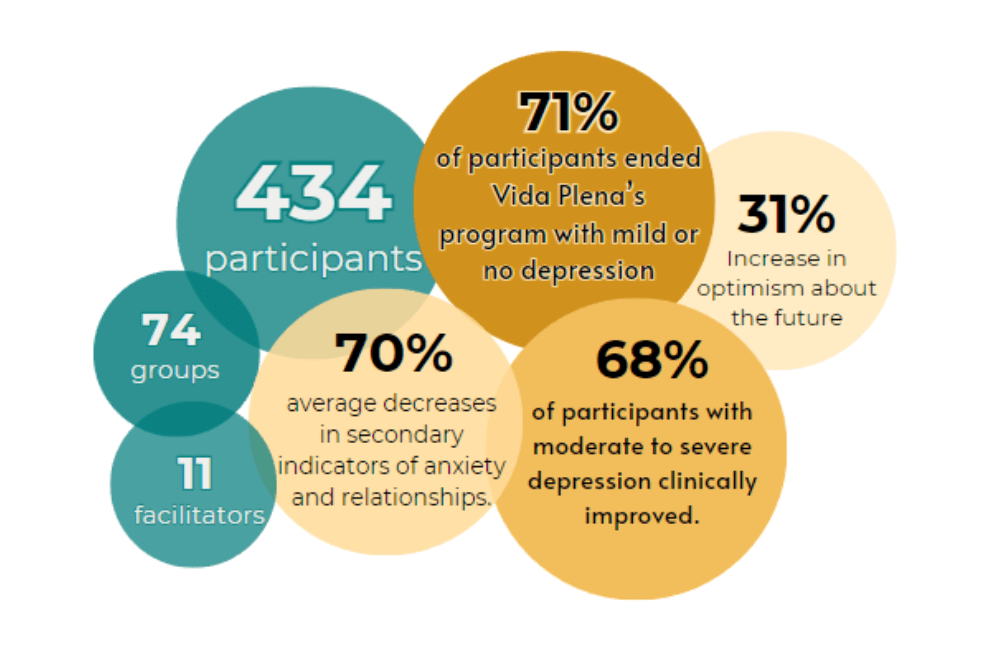
Since launching two years ago, we have been working to determine if the g-IPT model is effective in Ecuador. While a formal RTC was outside of the scope of our program for 2023, we analyzed our impact pre and post-treatment and found that 71% of participants ended our programming with mild or no depression, and 68% of participants with more severe depressive symptoms clinically improved, some of whom in just two weeks.
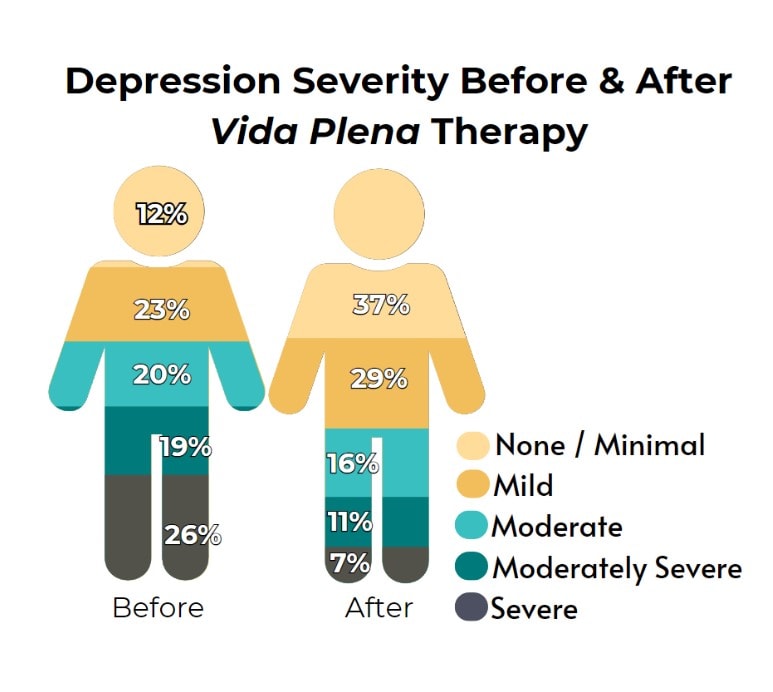
In 2023, nearly 55% of Vida Plena participants entered the program with thoughts of self-harm or suicide, even those with lower levels of depression. However, through our programming, participants saw a substantial reduction in these risks. Our internal analysis, supported by peer-reviewed studies, shows that participants in our g-IPT program recovered from depressive symptoms at rates far higher than those seen in spontaneous remission—the natural recovery some individuals experience without any treatment. This contrast underscores the effectiveness of our program helping participants achieve meaningful improvements in their mental health that would have been unlikely otherwise.
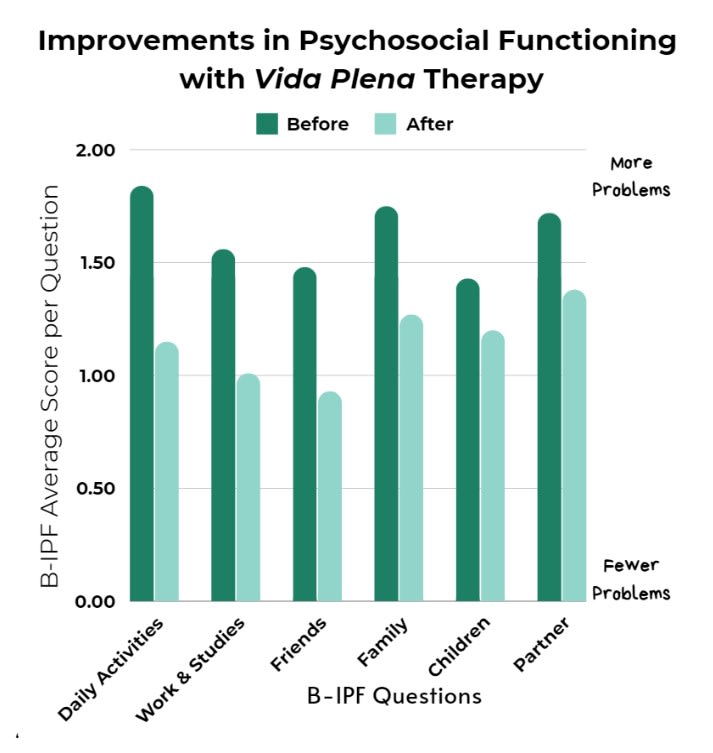
Our therapy doesn’t just assess depression but also helps provide tools for managing anxiety and improving wellbeing including repairing and maintaining healthy interpersonal relationships. Our 2023 results suggest that Vida Plena therapy helps with both anxiety and wellbeing as both assessments showed clinical improvement. Most importantly, participants having gone through our programming, report having regained hope (86%), having improved resilience (85%), and better overall functioning (85%). Our full analysis was disseminated in our 2023 annual report.
Our combined evidence suggests that Vida Plena actively does no harm and actively gives participants the tools they need to combat depression, foster resilience, and garner hope. Thus we are ready to vastly scale in 2025 with the help of two governmental agencies and to conduct a full RTC in 2026 and double the amount of people we can reach with g-IPT.

Cost-Effectiveness
Currently, it costs $233 for a participant to have eight weeks of g-IPT through Vida Plena with three follow-ups which is half the cost of private care.
Once operating fully at scale, we estimate that it will cost Vida Plena $462 to prevent one DALY.
However, we prefer measuring impact in well-being-adjusted life years (WELLBY), which gauges overall wellbeing, in contrast to DALYs’ focus on disease and disability. Using this metric, we estimate it costs $17 to enhance a person’s well-being by one WELLBY, making it eight times more cost-effective than the benchmark of direct cash transfers. See our predictive CEA for further details.
Vida Plena provides g-IPT at no cost to participants. In the areas where we work, mental health care—whether private or public—is out of reach for vulnerable populations due to high costs or lack of availability. Vida Plena was created to ensure that, regardless of economic status, location, or social standing, everyone has access to the mental and emotional tools needed not only to survive but to thrive.
Possible Reasons for Not Funding Vida Plena
- Impact Uncertainty: Our cost-effectiveness figures are projections, lacking local data for a control group (we aim to carry one out in 2026). Although our program's effectiveness is backed by other organizations' RCTs, results come with inherent uncertainties.
- Additionally, some readers might prefer DALYs over WELLBYs for cost comparisons, and therefore other initiatives will be more cost-effective.
How You Can Help:
Donate:
- If you'd like to support us, consider donating on our website. Donations are tax-deductible for US residents. For bigger contributions, let's chat! Drop an email to joy@vidaplena.global
Stay in Touch:
- Want to keep up with our work? Follow us on LinkedIn, Instagram, or subscribe to our newsletter.
Tell a Friend:
Know someone who'd be interested? Share our story! Whether it's this post, our website link, or encouraging them to join our newsletter, your recommendation matters.
Thanks for being part of our journey!



Hey team, thanks for sharing this update!
A few comments, not intended as a knock on Vida Plena's programme, but perhaps more relevant to how it's communicated:
Given this is the first bullet under "helping a life flourish" I thought this might benefit from some clarification, because the vast majority of the value of this programme is likely not from suicide prevention, given low absolute rates of suicide.
From the same source: "at two years, the cumulative hazard of suicide death ranged from 0.12% in young adults to 0.18% in older adults." Under unreasonably optimistic assumptions,[1] Vida Plena would prevent 1 suicide every 500 participants / prevent a suicide for $116,500, which is something between 21x to 39x less cost effective than GiveWell top charities.[2] More reasonable assumptions would drop this upper bound to 1 suicide prevented every ~1200 participants, or ~$272,000 per suicide prevented / ~50-90x less effective than GW top charities.[3]
Given you hope to reach 2,000 people by the end of 2025 for $50,000, this suggests a reasonable upper bound is something like 2 additional suicides prevented.[4]
This isn't a claim that the cost-effectiveness claims are necessarily incorrect, even with minimal suicide prevention. A quick sense check RE: $462/DALY and 0.22 DALYs per participant would imply that Vida Plena would need to more than halve their cost per participant (from $233 down to $101), and then achieve results comparable to "~100% of people with severe / moderate mild depression conclude the programme going down one level of severity or something like ~5 points on the PHQ9 score (severe --> moderate; moderate --> mild; mild --> no depression)."[5] This is well within your listed results - though as you note in your annual report these have some fairly significant sources of bias and (IMO) probably should not be taken at face value.
Some other comments:
Even if 100% (rather than 24%) of individuals were in the high risk group (i.e. suicidal ideation nearly every day), and even if you dropped 100% of individuals risk of suicide from 0.2% to zero (rather than reducing it by 3-11x or to baseline), and if this effect persisted forever rather than just the initial 30 days
233 * 500 / 3000 = 38.83
233 * 500 / 5500 = 21.18 (assuming 1 prevented suicide = 1 life saved)
If 24% of your participants were high risk (7x risk, at 0.18%), and the other 76% of them were half of that (3.5x risk, at 0.09%), and you successfully reduced 100% of participants to baseline (0.026%), you would prevent 1 suicide every 1169 participants, which comes to ~$272,000 per life saved, or ~50-90x less cost effective than GW top charities.
(0.18-0.026) * 0.24 + (0.09-0.026) * 0.76 = 0.0856
100 / 0.0856 = 1168.2
1168.2 * 233 = 272190.6
272190.6 / 3000 = 90.73
272190.6 / 5500 = 49.4892
It's also worth noting these are cumulative hazards at 2 years rather than 30, and the hazard ratios at 365 days are approximately halved compared to 30 days (1.7- to 5.7 instead of 3.3-10.8), so these figures are plausibly a few factors optimistic still.
Severe --> moderate depression is about 0.262 DALYs averted, moderate --> mild depression is about 0.251 DALYs averted, and mild --> no depression is about 0.145 DALYs averted.
HAP is described as "a psychological treatment based on behavioral activation...consist[ing] of 6 to 8 weekly sessions of 30 to 40 minutes each, delivered individually at participants’ homes or at the local PHC."
THPP is a simplified version of a psychological intervention (THP) for treating perinatal depression that has been found to be effective in similar settings and is recommended by the WHO (Rahman et al., 2008, 2013; WHO, 2015; Baranov et al., 2020). While the original THP trials employed a full-fledged cognitive behavioral therapy (CBT) intervention, THPP was a simpler intervention focused on behavioral activation, as in the HAP trial described above. THPP was designed to be delivered by peer counselors, instead of community health workers as in previous trials.
[taken from here, emphasis added]:
-Our findings add to this evidence base by showing 12-month modest improvements of 20%-30% in rates of minimal depression for adolescents assigned to IPT-G, with these effects completely dissipating by the 24-month follow-up. We similarly find small short-term impacts on school enrollment, delayed marriage, desired fertility and time preferences, but fail to conclude that these effects persist two years after therapy.
-Given impact estimates of a reduction in the prevalence of mild depression of 0.054 pp for a period of one year, it implies that the cost of the program per case of depression averted was nearly USD 916, or 2,670 in 2019 PPP terms.
-This implies that ultimately the program cost USD PPP (2019) 18,413 per DALY averted. (almost 8x Uganda's GDP per capita)
Hi Bruce, great to reconnect here! Thank you for all your thoughtful comments. I really appreciate your perspectives. Here are my responses to your points.
Yes, we are primarily a "life-improving" intervention rather than a life-saving one. While we do track suicidal ideation and believe we may have prevented several suicides, proving this counterfactually is challenging. So, when calculating our impact, we consider lives saved as a "bonus" rather than our primary measure of impact. As such, we don't account for that in our cost-effectiveness estimates.
We are on track to improve our cost per person (but still not there). The $233 cost per person reported for 2023 included our total spending for the year, which involved significant consulting fees to Columbia University for their supervision in our first year. Excluding those fees, which are not recurring, our actual cost per person was $152 in 2023. We expect 2024 to be in that range.
Regarding your other notes:
So appreciate the thoughtful feedback, it helps us to refine our thinking and keep improving!
Thanks for the response, and likewise - hope you've been well! (Sorry I wasn't sure if it was you or someone else on the account).
I agree that it is pretty reasonable to stick with the same benchmark, but I think this means it should be communicated accordingly, as VP are sometimes referring to a benchmark and other times referring to the GD programme, while GW are sticking to the same benchmark for their cost-effectiveness analyses, but updating their estimates of GD programmes.[1]
E.g. the predictive CEA (pg 7) referenced says:
"This means that a $1000 donation to Vida Plena would produce 58 WELLBYs, which is 8 times more cost-effective than GiveDirectly (a charity that excels in delivering cash transfers - simply giving people money - and a gold standard in effective altruism)"[2]
I think people would reasonably misinterpret this to mean you are referring to the GD programme, rather than the GW benchmark.[3] Again I know this is a v recent update and so hadn't expected it to be already updated! But just flagging this as a potential source of confusion in the future.
Separately, I just thought I'd register interest in a more up-to-date predictive CEA that comes before your planned 2026 analysis, in part because there's decent reason to do so (though I'm not making the stronger claim that this is more important than other things on your plate!), 2026 is a while away, and because it's plausibly decision relevant for potential donors if they're not sure the extent to which HLI updates might be applicable to VP.
"Thus, we will be using our historic benchmark until we have thought it through. For now, you can think of our benchmark as “GiveWell’s pre-2024 estimate of the impacts of cash transfers in Kenya,” with GiveDirectly’s current programs in various countries coming in at 3 to 4 times as cost-effective as that benchmark."
The summary table on the same page also just says "GiveDirectly".
To VP's credit, I think "eight times more cost-effective than the benchmark of direct cash transfers" in this post would likely be interpreted correctly in a high context setting (but I also think reasonably might not be, and so may still be worth clarifying).
I’m not sure about this; the HLI’s analysis of GiveDirectly only looks at direct individual effects and household spillovers. Whereas GiveWell’s update seemingly only found additional effects in terms of non-household spillovers, mortality, and consumption (based on a 5 minute check, so I might be wrong here).
I think it’s reasonable to argue that depression prevention would also have effects on mortality, consumption (via productivity increases—my guesses here peg this quite high, especially in LMICs and UMICs), and non-household spillovers (via increased income being reinvested into communities, using the same mechanism as GD). Unless there’s reason to believe that the non-accounted-for impacts on WELLBYs systematically favour GiveDirectly I’d be cautious about applying a discount—but curious for your take on that :)
I might be misunderstanding you, but are you saying that after reading the GD updates, we should update on VP equally to GD / that we should expect the relative cost-effectiveness ratio between the two to remain the same?
Hmm, no. I wouldn’t want Vida Plena to update without evidence that they have those secondary effects.
But I think it would also be misleading to compare direct effects + household spillovers (in the case of Vida Plena) to direct effects + household spillovers + community spillovers + mortality reduction + consumption increases (GiveDirectly), unless you had good reason to believe that Vida Plena’s secondary effects are much worse than GiveDirectly’s. So I suppose I would be wary of saying that GiveDirectly now have 3–4x the WELLBY impact relative to Vida Plena—or even to say that GiveDirectly have any more WELLBY impact relative to Vida Plena—without having a good sense of how Vida Plena performs on those secondary outcomes. (But I feel like maybe I’m misunderstanding what you meant by applying a discount?)
Ah right - yeah I'm not making either of these claims, I'm just saying that if the previous claim (from VP's predictive CEA) was that: "Vida Plena...is 8 times more cost-effective than GiveDirectly", and GD has since been updated to 3-4x more cost-effective than it was compared to the time the predictive CEA was published, we should discount the 8x claim downwards somewhat (but not necessarily by 3-4x).
thoughtful comment! just want to throw in that suicide should not be considered in isolation imo. while every avoidable death is horrible ofc, I do think that suicide has particularly bad knock-on effects.
Just a quick comment-- I think this is a really creative idea for an infographic- love it. Especially when supplemented with the graph with more info that you included.
thanks so much! Love having a creative team!
Yeah me too its amazing
thanks so much, Nick!