I was wondering, how useful would a short write up of 'Could far UVC have averted histories deadliest pandemics' be? I expect it would take me about 2-3 hours for a rough write up, rising to about 5 hours to include some meaningful graphics. I've done research into the types of pathogens and which ones are likely to be effected by far UVC, and also which have more or less chance of resistance/adulteration. E.g. if 90% of the most deadliest pandemics (e.g. top 10) in the last few centuries could have been avoided, it would signal for example some level of confidence natural pandemics would be reduced from X/S-risk if we had it, vs if only say 10% of pandemic candidate pathogens are meaningfully affected by far UVC, it points to is more as a business/sick leave cost reduction rather than meaningful government/organisational broad scope pandemic protection? I'd analyse trends in also future pathogen candidates e.g. H5, H1 (swine, avian) plus whether malicious threat actors are likely to utilise heavier/lower weight pathogens e.g. fungi/bacteria vs viruses/spores etc (but unsure if that part I will publicly post)
I've been doing some data crunching, and I know mortality records are flawed, but can anyone give feedback on this claim:
Nearly 5% of all deaths (1 in 20) in the entire world occur from direct primary causation recorded due to just 2 bacterial species, S. Aureus and S. Pneumoniae.
I'm doing a far UVC write up on whether it could have averted history's deadliest pandemics. Below is a snippet of my reasoning when defining 'CURRENT' trends in s-risk bio.
Analysis of pathogen differentials:
2021-2024 data: Sources Our World in Data, Bill and Melinda Gates Foundation, CDC, FluStats, WHO, 80 000 hours
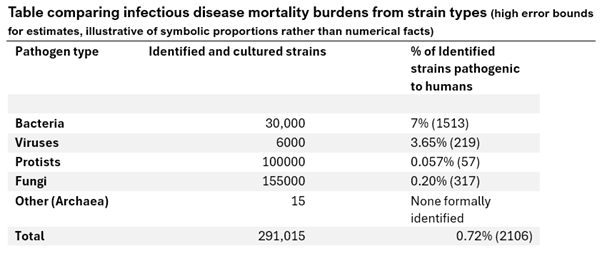
Figure 8: Comparison of number of identified and cultured strains of pathogen types
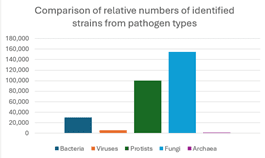
Figure 9: Comparison of number of strains pathogenic to humans by pathogen types
From the data, despite a considerable amount of identified strains of fungi and protists, the percentage of the strains of those pathogen types that can pose a threat to humans is low (0.2% and 0.057%) so the absolute amount of strains pathogenic to humans from different pathogen types remains similar to viruses, and becomes outweighed by pathogenic bacteria.
Archaea have yet to be identified as posing any pathogenic potential for humans, however, a limitation is that identification is sparse and candidates of extremophile domains tend to be less suitable for laboratory culture conditions.
The burden of human pathogenic disease appears clustered from a small minority of strains of bacterial, viral, fungal and Protoctista origin.
Furthermore, interventions can be asymmetrical in efficacy. Viral particles tend to be much smaller than bacterial or droplet based aerosols, so airborne viral infections such as measles would spread much quicker in indoor spaces and would not be meaningfully prevented by typical surgical mask filters. Whilst heavy droplet particles or bodily fluid transmission such as of colds or HIV can be more effectively prevented by commercial masks or barrier contraception.
Interventions aren’t always exclusive though, for example, Far UVC can reduce light viral particles that are not filtered by public masks, and droplets that are too large for UVC inactivation can be caught by the mask filter. However, the difference in occupant participation, risk perception, cost and cultural norms can make individuals favour one intervention as an exclusive solution.
However, further analysis into health outcomes between incidence of exposure, incidence of ill health, health resource strain and morbidity is useful to identify types and groups of sub strains that are responsible, and the differences in S-risk and X-risk potentials.
S risks include pathogens likely to cause a large scope of illness in a large amount of individuals such as the common cold, without considerable high death rates. The tractability of preventing each infection is harder the more transmissible the pathogen is, however the lethality is much lower than other pathogens.
Another S risk could be a highly lethal but not very transmissible pathogen such as Ebola, which despite causing suffering and very poor health outcomes, is not likely to cause widespread global death or disease burdens or lead to international collapse at its current virality.
X-risk candidates are a controversial definition but contain themes of societal collapse, worldwide economic repercussions, apocalyptic levels of deaths, and healthcare strain that results in high excess deaths or disability. These could include, but are not limited to, highly infectious strains of Influenza (Swine and Avian variants, Spanish Flu 1918 serotype), diseases such as poliovirus and XDR-Tuberculosis, measles and smallpox viruses (due to high incubation and shedding), HIV/AIDS, severe malnutrition related instances, and mosquito borne diseases (namely malaria).
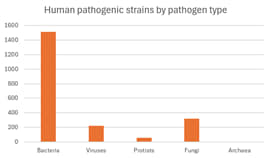
Non communicable diseases have now surpassed diarrhoeal, parasitic and infectious disease deaths and negative health outcomes in most HICs. Cancer and cardiovascular disease is now the most common cause of death worldwide, whilst over 10 million of the 14.8 million annual worldwide primary infectious disease deaths occur in just one continent (Africa). This highlights how infectious disease burdens are not felt equally.
Many preventable diseases such as Tuberculosis, Polio, Measles and more can be reduced, eliminated or prevented with vaccination, nutrition programs, sanitation systems, and appropriate access to medicines.
However, international aid efforts can be hampered by lack of access or acceptance, stigma, budget deficits, lack of record keeping and geographic isolation.
Plus underreporting of LIC infectious causes of death can allow for emerging zoonosis and pathogens to reach epidemic status before appropriate surveillance and emergency containment responses.
Infectious diseases tend to be cheaper, quicker and more likely to be eradicated or prevented if caught early, especially pathogens with high reproduction numbers and those with a propensity to accumulate advantageous chance mutations.
It is expected many diseases can mutate to increase or decrease the likelihood of pathogenic pandemic potential, however certain characteristics such as asymptomatic spread during incubation, moderate death rates, high transmissibility, immunity amnesia, vague symptoms, and multi systemic receptor mediated reproduction can create biorisk threat axis of natural or engineered origin by certain pathogens.
On the flipside, pathogenic candidates suitable for eradication or reduction share characteristics including distinguishable symptoms, lack of pre-symptomatic spread, lack of animal reservoirs and low mutation rates which can allow for immunisation or quarantine campaigns, such as with Smallpox or Rinderpest.
With this in mind, an analysis of certain pathogen types and strains as linked to current annual global primary cause of death on record could allow for crude comparison of current and historical trends of pathogen instance.
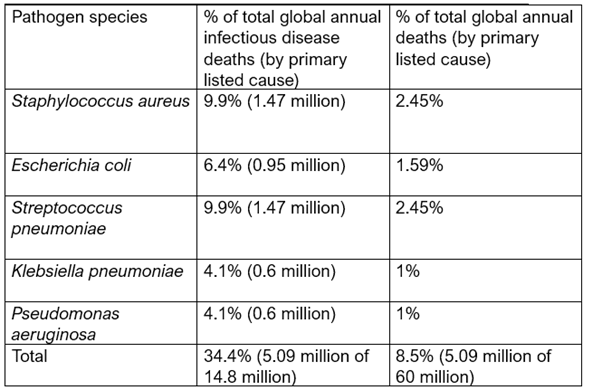
When weighted for deaths per strain over 50% of all bacterial infection attributed deaths (>3.5 million annually) occur from just 5 species:
– Staphylococcus aureus
– Escherichia coli
– Streptococcus pneumoniae
– Klebsiella pneumoniae
– Pseudomonas aeruginosa
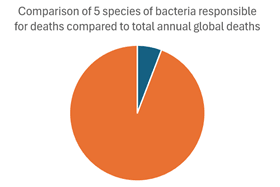
These 5 species account for over 3.5 million of 60 million total global deaths from all causes, and are responsible for around 1 in 15 recorded primary causes of death.
Death counts are an incomplete metric of disease and strain burdens, since there can be many contributing factors, and record keeping and accuracy fluctuates, especially during periods of high fatality.
The burdens of infectious strains of all pathogens appear similar in absolute number, but have differential risk of exposure, illness and mortality.
However, the burden of morbid outcomes from bacterial pathogens greatly outnumber viral, fungal, and Protoctista.
This suggests that far UVC to reduce mortality and mass pathogen exposure should be effaceable against bacteria (namely the 5 most common species) and certain viruses. However, instead of broad generalisation, an analysis of the most common pathogenic and pandemic-causative bacterial and viral pathogens seems pertinent.
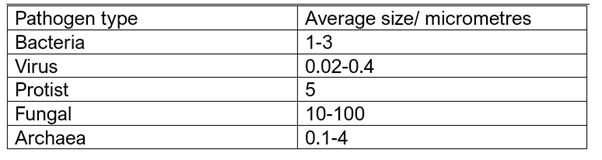
The above table demonstrates the range of average diameter of pathogenic types in micrometres. Far UVC tends to be considerably more effective at lighter and smaller particle inactivation, and the previous analysis demonstrating the 5 most mortality-associated pathogens globally are all clustered in the bacterial domain.
If accounting for the most common mortality associated pathogens, the following 5 bacterial species are compared:
The two most common species linked to mortality are:
– Staphylococcus aureus
– Streptococcus pneumoniae
Jointly accountable for around 2.94 million deaths per year globally, with 19.8% of all infectious disease attributed deaths being directly listed as caused by those two species. The number of deaths also encompasses 4.9% of all global annual deaths recorded of any cause worldwide.
To emphasise:
Nearly 5% of all deaths (1 in 20) in the entire world occur from direct primary causation recorded due to just 2 bacterial species, S. Aureus and S. Pneumoniae.
These will be the two species explored for S-risk reduction in far UVC susceptibility
The recent pivot by 80 000 hours to focus on AI seems (potentially) justified, but the lack of transparency and input makes me feel wary.
TLDR;
80 000 hours, a once cause-agnostic broad scope introductory resource (with career guides, career coaching, online blogs, podcasts) has decided to focus on upskilling and producing content focused on AGI risk, AI alignment and an AI-transformed world.
According to their post, they will still host the backlog of content on non AGI causes, but may not promote or feature it. They also say a rough 80% of new podcasts and content will be AGI focused, and other cause areas such as Nuclear Risk and Biosecurity may have to be scoped by other organisations.
Whilst I cannot claim to have in depth knowledge of robust norms in such shifts, or in AI specifically, I would set aside the actual claims for the shift, and instead focus on the potential friction in how the change was communicated.
To my knowledge, (please correct me), no public information or consultation was made beforehand, and I had no prewarning of this change. Organisations such as 80 000 hours may not owe this amount of openness, but since it is a value heavily emphasises in EA, it seems slightly alienating.
Furthermore, the actual change may not be so dramatic, but it has left me grappling with the thought that other mass organisations could just as quickly pivot. This isn't necessarily inherently bad, and has advantageous signalling of being 'with the times' and 'putting our money where our mouth is' in terms of cause area risks. However, in an evidence based framework, surely at least some heads up would go a long way in reducing short-term confusion or gaps.
Many introductory programs and fellowships utilise 80k resources, and sometimes as embeds rather than as standalone resources. Despite claiming the backlog content will remain, I see some potential disincentive to take on the resource-intensive linkrot and resource integrity work that they require, leading to loss of information and patchy dissemination.
I also use 80k as a cause agnostic introduction to many new EAs, especially at my university group. Career advising and resources focused on AI on impressionable young people can lead to lack of choice and autonomy, feelings of pressure, alienation and more. I can also see the very claim of 'work on AI as it's a big risk!' to be widely contested in and of itself, let alone the idea a key stakeholder in the EA community should endorse a lone cause so strongly.
The change may be positive, and has been met with some support, but the infrastructure in place to ensure the community is involved seems lacking. We may not have a duty to involve everyone, nor should we try to get total unanimity, but surely the values of EA would be supportive of at least some more shared decision making?
Some concrete pitfalls that I would appreciate discussion on:
- Is a short (mainly unseen) post enough to justify/communicate the change?
- Do they even owe justification?
- Should this have been discussed before the change?
- How can information content on non-AGI be safely preserved for linked resources?
- What resources (e.g. probably good) can take the place?
- Do they have enough runway to patch the gap?
- With sudden shifts in Bluedot (less biosec, focus on AI), Rethink Priorities, Atlas and other high school outreach, CEA and OP ceasing U18 and uni organiser funding, EA funds and EV changing main scopes etc- what safeguards (or should there even be safeguards) are in place in the community to prevent sudden upheaval
- Does this signal a further divide between longermists/X-risk rationalists and the more concrete level health/biosec/nuclear/welfare EA community?
Finally, the least knowledgable aspect I would appreciate clarification on is:
Should we actually all shift to considering direct AI alignment work over just reassessing what risks change in an AGI impacted future?
I know 80k aren't claiming direct AI work for all is the 'correct' choice, but it surely incentivises a 'norm' pro AI cause area work.
I see some issues adapted from an anecdotal reasoning. I appreciate AI may be a higher X risk and may be increasing in scale and impact, but compared to S-risks from pandemics or health/biology impacts, I see more tangible routes for good (maybe because I'm more risk averse) plus higher chance of suffering even if it is smaller in scale that leads to nearly as great overall expected risk.
E.g. multiple deaths from preventable diseases compounding to be nearly the same as entire society value lock in my misaligned AI... (in my naive view)
Plus, AI focus doesn't account for interest or personal experience, there's diminishing returns of mass career shifts and dilution of roles and zero sum grant funding to less advantageous candidates who feel forced into it... It's an extreme but also seems like 80k holds a big generalist pull and lot of norm setting power, so is something to bear in mind with how this may affect smaller entities and orgs.

This seems like a great post to exist!