TLDR: The best research we have shows that clean water may provide a 30% mortality reduction to children under 5. This might be the biggest mortality reduction of any single global health intervention, yet we don’t fully understand why it works.
Here I share my exploration of a life-saving intervention that we don’t fully understand, but really should. I may err a little on the side of artistic license - so if you find inaccuracies or I'm a bit loose please forgive me, correct me or even feel free to just tear me to shreds in the comments ;).
Part 1: Givewell’s Seemingly absurd numbers
I first became curious after a glance at what seemed like a dubious GiveWell funded project. A $450,000 dollar scoping grant for water chlorination in Rwanda? This didn’t make intuitive sense to me.
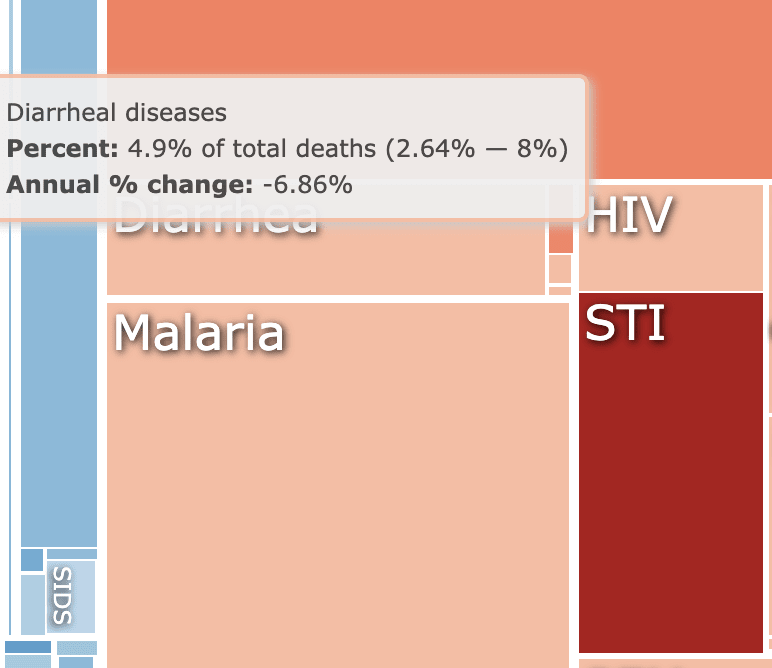
In Sub-saharan Africa diarrhoea causes 5-10% of child mortality. While significant, the diarrhea problem continues to improve with better access to medical care, improving ORS and Zinc coverage, and antibiotics for more severe cases. Over the last 5 years, our own Ugandan health centers have encountered surprisingly few very sick kids with diarrhoea and I’ve hardly seen diarrhoea kill a child, as opposed to Malaria and Pneumonia which tragically kill kids all the time. It seemed to me that even if clean water hugely reduced diarrhoea mortality, the intervention would still likely be an expensive way to achieve 1 or 2 percent mortality reduction,
So with my skeptic hat on, I clicked the GiveWell spreadsheet and my incredulity only grew. GiveWell estimated an upper-bound mortality reduction of an almighty 17% for the Rwandan chlorination program! At first that made no sense, but I did expect GiveWell would likely be lesswrong than me.
The Global burden of disease estimates that Diarrhoea makes up only 4.9% of total deaths in Rwanda. How could an intervention which targets diarrhoea reduce mortality by over three times the total diarrhoea mortality? Even if the clean water cured all diarrhoea, that wouldn’t come close to GiveWell’s mortality reduction estimate.
Something fishy was afoot, but I quickly found some answers, through a nobel prize winner’s study which was partially funded by you guessed it…….. GiveWell
Part 2: A Nobel Prize winner’s innovative math
Michael Kremer won a Nobel prize along with two J-PAL co-founders for their wonderful work pioneering randomised controlled trials to assess development interventions. What better person to try their hand at estimating the mortality benefit of clean water than a father of the RCT movement?
But connecting clean water and mortality is tricky, because to date no-one has actually asked whether clean water can reduce child mortality. Instead, a number of RCT asked the more obvious question, does clean water reduce diarrhoea. The answer obviously yes.
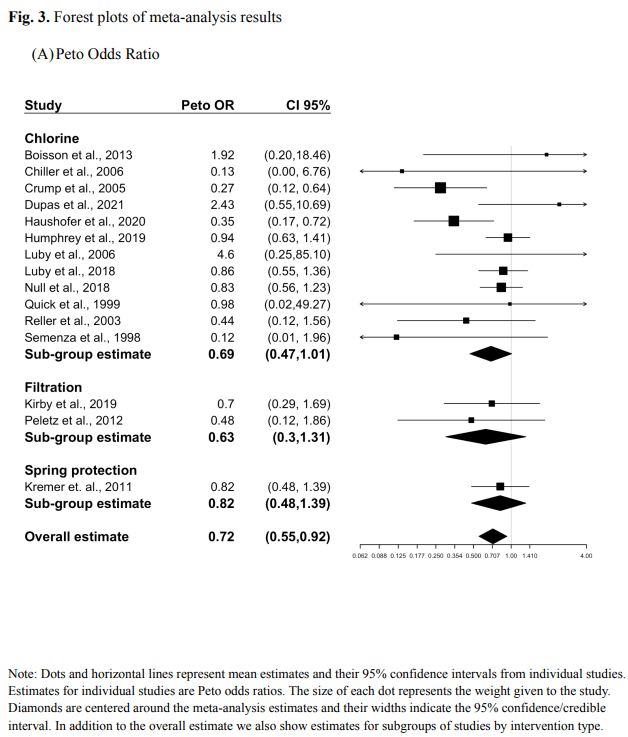
But Kremer and co. found a clever way around this. They sifted through all studies which looked at the relationship between clean water and diarrhoea and identified 12 studies[1] that also gathered bits and pieces of mortality data. They then performed a meta-analysis, pooling that mortality data together to see whether clean water save kids’ lives.
The result – they estimated that clean water caused an incredible 30% mortality reduction in kids under 5. If this is even in the ballpark of correct, clean water could could prevent one in three childhood deaths in much of sub-saharan Africa. If Africa could chlorinate and filter all drinking water, we could save perhaps 1 million lives every year in sub-saharan Africa alone. Mosquito nets might bow to their new king.
To be as crystal clear as the water, this is not just a 30% reduction in diarrheal deaths, but a 30% reduction in overall under 5 mortality. To put this in perspective, mosquito nets reduce childhood mortality by about 20% [2] and in one smallish study the new R21 malaria vaccine RTS,S was associated with an estimated 13% mortality reduction [3] This raises a fairly obvious question.
How does clean water cause that almighty mortality reduction?
Because it ain’t just the diarrhea. Kremer and co calculated that reduction in diarrhoea deaths account ed for only 1 in 8 of the lives saved by the clean water intervention.
Part 3. We already knew about this anomaly – 100 years ago
It turns out that science has been around for quite some time, and sometimes the scientific-wheel-of-time comes full circle. Over 100 years ago, this exact same phenomenon Kremer observed in 2023, was independently discovered by two scientists on opposite sides of the world - Mills in Lawrence, USA and Reinke in Hamburg, Germany.
In the late 19th century Germany and the USA finally began systematically filtering their water – for the first time huge swathes of the western world drank, bathed and washed clothes with water cleared of microbial soup. As expected the horrible killer that was typhoid was all but wiped out, but Mills and Reinke noticed something more profound - Childhood mortality plummeted, far more than could be explained by the absence of typhoid. Some reports claimed a 40%, or even 50% drop in child mortality. The world all of a sudden became a whole lot better than we expected.
In a landmark 1910 paper [4] this anomaly was labelled The Mills- Reinke Phenomenon in a widely cited paper by Sedgewick, another public health legend. As I write this in Boston after the EAG, I feel some warm fuzzy local MIT history.
Part 4: But why?
Occam’s razor suggests that the reduction in mortality might be due to reduction in a range of non-diarrhoea infectious diseases as well. Perhaps when people wash with clean water, bugs that cause disease such as pneumonia and meningitis are killed and don’t spread as readily as before. Perhaps neonatal infections are reduced as cleaner water is used in the birthing process.
Or maybe its something different - when the body stops taking hits from diarrhoea, malnutrition reduces and the immune system can handle other infections better. This is more likely than you might think, as without clean water kids get diarrhoea all the time, in the ballpark of 5 times [5] each year.
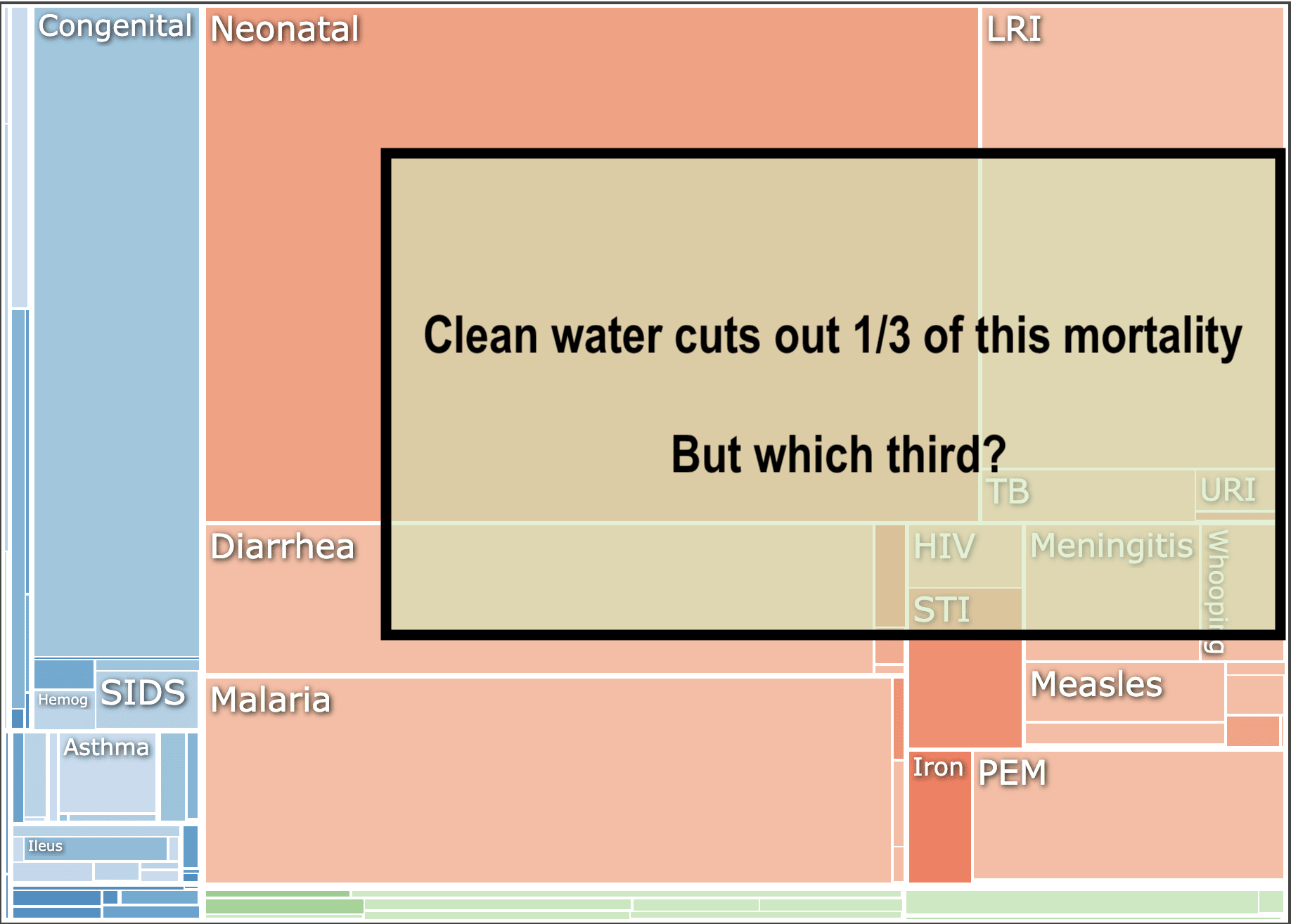
However even if we add together a bunch of potential infectious disease reductions, it is not easy to explain a full 30% mortality benefit. To visualize this, here’s GBD’s causes of under 5 mortality in Rwanda and how much of the square we would need to cut out to account for a 30% reduction.
To demonstrate how hard it is to account for this mortality reduction, here's an example of a barely plausible "lolly bag" of mortality reductions that we would need to account for even a 25% total mortality reduction
- 50% reduction in diarrhea mortality (at the extreme end of what is reported in studies)
- 30% reduction in neonatal mortality
- 30% reduction in pneumonia mortality
- 50% reduction in Malnutrition mortality
- 20% reduction in malaria mortality (from improved immunity and nutrition? Clean water can't plausibly reduce malaria prevalence as mosquitos don't care how clean your skin or gut are)
Perhaps you have a better, novel idea of how this all works, can prove it and win the Nobel prize. You might collect it hand in hand with Kremer as he receives his second…
I suppose one could argue that “the why” isn’t so important. What matters is the benefit, the consequences. We should pass go, collect the fantastic mortality reduction and "wash our hands"[6] of the question. I disagree – understanding the science here might reveal other hidden benefits. It may help us choose better between different methods of cleaning the water. Or if there is immunology involved, we might even be pointed towards new vaccine techniques or other solutions for infectious diseases.
This mystery should be solved.
Part 5: What next for clean water?
1. We still need a RCT powered for Mortality
This may seem like overcaution, but I don’t think our data is good enough yet to call the slam-dunk on clean water as this apparently epic magic bullet for reducing child mortality. Kremer looks retrospectively at data not gathered for-purpose, which is in epidemiological speak a little dodgy. As of yet, we have no RCT which has been designed and powered to detect mortality benefits from clean water. I have heard there may be a study underway looking at this, but I couldn’t find it (let me know if you can). If it is ongoing, I sure hope they are looking at the causes of excess mortality in the non-clean water group, because that could get us a lot closer to understanding the why.
2. We should (probably) continue scaling up clean water in the meantime.
The data we have strongly suggests that cleaning water is likely to be a high cost-effective intervention. A bigger practical debate may be how to clean the water. Evidence Action’s large scale program uses multiple methods, including water dispensers for individual households and in-line chlorination. However given that these are not permanent measures there is a reasonable more long-termist[7] argument that simply speeding up the expansion of nationwide piped water networks might be a more durable, longterm approach albeit more expensive and slow.
3. WE NEED TO KNOW WHY lives are being lost from dirty water, and saved by the clean stuff. Is it mostly due to one disease? From a range of diseases? From something else entirely? If we understand why, this may open up other avenues and interventions which could save further lives. We owe it to great scientists like Kremer, Mills, Reinke and Sedgewick, but even more to the millions of kids still dying every year because they aren’t drinking clean water.
- ^
Only 5 of these were RCTs. Givewell's more conservative 17% number arose from leaving out the other studies, and only using the RCTs in their analysis
- ^
- ^
https://www.science.org/content/article/first-malaria-vaccine-slashes-early-childhood-deaths
This 13% mortality reduction from the malaria vaccine also doesn't make complete sense, when malaria only makes up about 10% of childhood mortality. Perhaps another article for another day... Maybe if we find enough interventions which massively reduce childhood mortality we could end up with negative mortality? (J/K)

I do work in this academic neighborhood, so maybe I’ll comment a bit. There’s a part of me that feels like caricaturing Linch’s question as akin to asking: What were all the other physicists doing with their time in 1905, when Einstein was sitting around churning out paradigm-shifting papers without a PhD or even access to a decent academic library? But that’s probably unhelpful, so I’ll try to give a bit more color on Kremer’s context.
First, it’s important to understand that until very recently, experimental work in LMIC settings was really prohibitively difficult to 1) organize and 2) get funded. Prior to the founding and (recently explosive) growth of the J-PAL/IPA network (in which Kremer himself played no small part), as well as the emergence of the Gates Foundation as a major funder of global health RCTs, these studies were just really, really hard to do. Moreover, even if you could put one together, until the last 10-15 years, you were very unlikely to be able to publish your results in a top-5 economics journal (and top-10 economics departments assess their tenure-track faculty almost exclusively on the basis of their publications in top-5 economics journals). If you look at Duflo’s early work on healthcare in India, a lot of it published, well, badly, by the standards of the MIT Economics Department. Miguel & Kremer's original deworming paper did make a top-5 journal (Econometrica), but only because they spun their contribution as principally methodological in nature. The title is “Worms: Identifying Impacts on Education and Health in the Presence of Treatment Externalities;” the paper basically pretends to be about approaches to accounting for potential interference/spillovers between treated and untreated units in an experiment, rather than about deworming itself. I’m too young, but folks I know who were around those circles at the time recall being told that empirical research on health in LMICs “wasn’t economics,” that it was “just reduced-form” and that committing to it was a terrible professional decision. This assessment of the professional consequences wasn’t without justification, either. Seema Jayachandran was denied tenure at Stanford as recently as 2011 due to prejudice against this sort of research. What Banerjee, Duflo, and Kremer won the Nobel for, more than anything else, was changing the field’s conception of what counts as economics in a fairly dramatic way.
So how did folks like Banerjee, Duflo, Kremer, Karlan, Miguel, etc. overcome those obstacles? In the cases of Banerjee and Kremer, both had established themselves as theorists (and received tenure at MIT) before they turned to doing experimental work. In the cases of Duflo, Karlan, and Miguel, 1) they were Banerjee/Kremer students, so they had access to that source of encouragement and support, and 2) they were unusually principled about their interests and willing to take gigantic professional risks.
The consequence of this is that those five names—in one permutation or another—are on a huge proportion of the papers evaluating health & development interventions with credible identification that were published prior to ~2010, and as for interventions that were first evaluated more recently, well, 1) the evidence base about those interventions is often still too thin to be the basis of a GiveWell recommendation, and 2) running these RCTs may be easier today than it was 20 years ago, but it’s still administratively challenging and (more importantly) difficult to fund. If you’re going to persuade Gates (or someone similar) to give you a seven- (or eight-) figure sum of money to figure out if sending people text messages gets them to vaccinate their children, it really helps if you can say that you’ll be drawing on someone like Michael Kremer’s network and expertise in putting your study together. This isn’t just empty signaling, either. There’s a lot that can go wrong in organizing an RCT like this, and having someone on the study team who has loads of experience navigating the challenges that tend to arise is genuinely very valuable. Moreover, if you’re a junior researcher, you may need someone like Kremer’s network in order to get the approvals you need to launch your intervention from the government wherever you’re working, to access J-PAL/IPA resources in-country, and to connect with other reliable implementation partners on the ground (e.g., local non-profits, survey firms, etc.).
In conjunction with the fact that Banerjee, Duflo, Kremer, Karlan, Miguel have all skyrocketed to (global) prominence in the last 15 years, this means that much of the best (particularly experimental) work happening in health and development even today still has one of their names on it. The best work, after all, requires a lot of money and excellent contacts, and the distinguished stature of those five economists has left them with money and contacts in spades. If you go on Kremer’s lab’s website, you can see that it employs, like, a shocking number of people (for a social science research center in a university setting). His personal contribution to the clean water paper under discussion here was probably not enormous, but it’s nonetheless no coincidence that he led it. If I’m a promising young economist with ambitions to do impactful work on these topics, then Kremer is going to be among the people I’d be most eager to collaborate with; I'm going to do everything I can to build a working relationship with him (especially given that he is also, reputedly, a nice guy). I think that's why you see him behind so many of GiveWell's recs.